The role of oxidative stress in DME
Throughout the body, any source of cellular damage (e.g., inflammation, infection, smoking, or high blood sugar) can liberate reactive oxygen species and set in motion an oxidative stress chain reaction that ultimately leads to tissue damage and pathology.
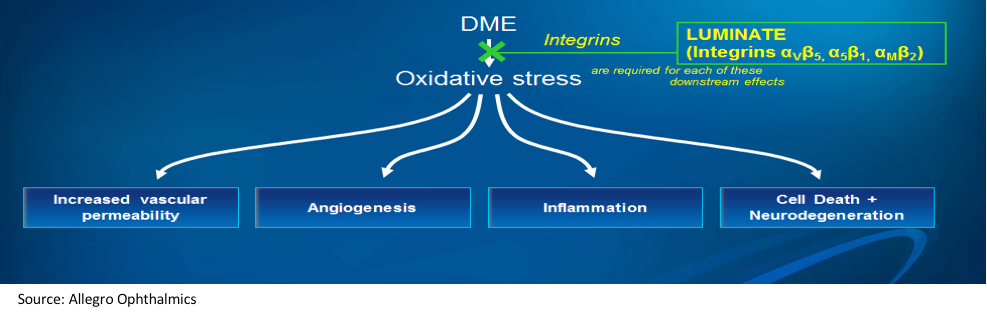
In retinal diseases, including diabetic macular edema (DME), oxidative stress activates multiple downstream pathways: increased vascular permeability; angiogenesis; inflammation; and apoptosis and neurodegeneration. These pathways may all be activated simultaneously-or their involvement may vary, depending on the individual patient and the disease stage.
Ophthalmologists are fortunate to have effective medications that address some of these pathways. Anti-VEGF agents target vascular permeability and angiogenesis, while steroids can address inflammation. However, there are no currently available agents that address all four pathways at once, and none that are neuroprotective.
Moreover, current therapies are insufficient-about 50% of DME patients still have edema after 1 year of anti-VEGF treatment.1
Even with state-of-the art therapies, patients may have continued leakage and/or vision that does not improve as much as ophthalmologists would like. It is possible that in these under- or non-responding patients, the VEGF-mediated pathways are not the primary pathways of damage.
Pipeline developments
Because of this need for new drugs to help the other 50% of patients with DME, there are many agents in the research and development pipeline. These include newer-generation anti-VEGF therapies that may be more effective or longer lasting than current agents, and combination drugs that combine anti-VEGF with a second drug targeting another pathway, such as Genentech's anti VEGF/ANG-2 combination therapy (RG7716), which has shown evidence of a longer duration of action and slight improvement of efficacy in phase II studies.
There are a number of monotherapy agents with non-VEGF targets, such as ANG-2 or PDGF inhibitors, Tie-2 activators, and KalVista Pharmaceuticals' KVD-001, a protease inhibitor that targets plasma kallikrein.
Other companies are working on new methods of delivery, such as suprachoroidal injection of steroids. Aerpio has been studying subcutaneous delivery of its Tie-2 activator, AKB-9778. Stealth Biotherapeutics has also explored subcutaneous injection (among other methods of delivery) of elamipretide, a mitochondrial therapy.
However, many of these new agents still target downstream effects of oxidative stress.
One new class of drugs, RGD class anti-integrin therapy, is appealing because it acts further upstream, with the potential to prevent oxidative stress pathways from being activated in the first place and therefore address all four oxidative stress pathways at the same time.
(Figure 1) Anti-integrin therapy (Luminate) targets integrin receptors to block oxidative stress upstream, before it has a chance to initiate multiple pathways implicated in DME. (Figure courtesy of Allegro)
Anti-integrin therapy
Integrins are cell adhesion and cell signaling receptors that have been associated with retinal disease as well as several systemic disorders. Anti-integrin therapy is currently in use to treat multiple sclerosis, Crohn's disease and colitis, thrombotic complications, and even signs and symptoms of dry eye.
SciFluor Life Sciences is developing a topical anti-integrin therapy for DME and wet age-related macular degeneration. This agent, SF0166, selectively inhibits the αVβ3 integrin receptor. Early clinical studies have demonstrated safety and a biological response, which helps to verify the validity of anti-integrin therapy. However, targeting only one integrin receptor may not inhibit all pathways of oxidative stress.
Further along in clinical development is Allegro Ophthalmics' first-in-class integrin peptide therapy, risuteganib (Luminate).
This therapy targets three integrin receptors that have been implicated in retinal disease, giving it the potential for broad-spectrum effects on oxidative stress (Figure 1). To date, there have been 1,150 human exposures to these anti-integrin therapy injections in more than 370 patients with no drug-related adverse events, so the safety of the drug is well-established.
(Figure 2) When all patients from the two studies were combined, both groups had similar gains in vision at Week 20. However, a different picture emerges when considering prior therapy. Treatment-naive patients had smaller vision gains with the anti-integrin therapy, while poor responders to anti-VEGF therapy had greater gains with the anti-integrin therapy compared with bevacizumab. (Figure courtesy of Allegro)
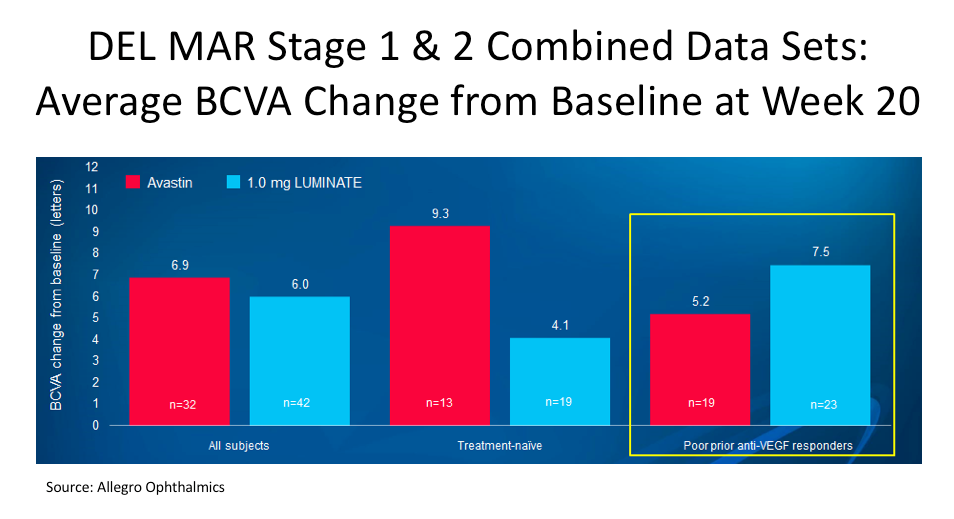
Two phase IIb DME studies have been completed and a phase III trial will be initiated in late 2018. This anti-integrin therapy was shown to be equivalent (in terms of vision and reduction in central macular thickness) to bevacizumab (Avastin, Genentech) at Week 20, with half as many doses, when used as monotherapy.
Pre-treatment with bevacizumab, followed by three monthly doses of this anti-integrin therapy (sequential therapy) was also equivalent to monthly bevacizumab therapy, although the two drugs given in combination were not effective.
Interestingly, the subjects who fared best with this anti-integrin therapy in these studies were those who had previously been poor responders to anti-VEGF therapy (Figure 2), which suggests that this anti-integrin therapy may be targeting other oxidative pathways that are more dominant than VEGF in these particular patients' disease.
Impact of anti-integrin therapy on oxidative stress
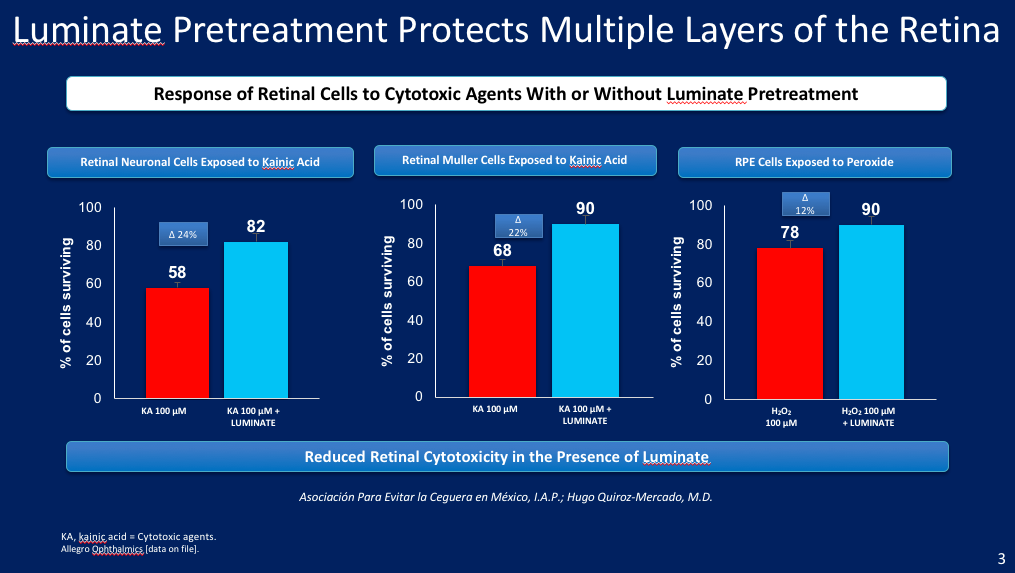
(Figure 3) Cells from several layers of the retina demonstrated reduced cytotoxicity when pre-treated with the anti-integrin therapy prior to kainic acid or peroxide exposure. (Figure courtesy of Allegro)
These clinical results are supported by a number of animal studies that provide evidence of the anti-integrin therapy's effect on each of the downstream oxidative stress pathways.
For example, Peter Campochiaro, MD, demonstrated a meaningful downregulation of angiogenesis with the anti-integrin therapy in ischemic, retinopathy of prematurity (ROP) mice. The drug was compared with anti-VEGF therapy and a control vehicle solution.
Dr. Campochiaro and Julie Kornfield, PhD, found that by downregulating integrin αMβ2, the anti-integrin therapy reduced leukocyte attachment and trans-epithelial migration, as well as reducing expression of Complement 3, an important immune system protein that is increased in response to inflammation.
Perhaps most exciting are data from several different groups of independent researchers that seem to demonstrate a consistent neuroprotective effect of the anti-integrin therapy. Most of this research is very new and not yet published. Hugo Quiroz-Mercado, MD, and colleagues in Mexico showed that pre-treating retinal tissues with the anti-integrin agent protected them from damage when they were later exposed to neurotoxins such as kainic acid and peroxide (Figure 3).
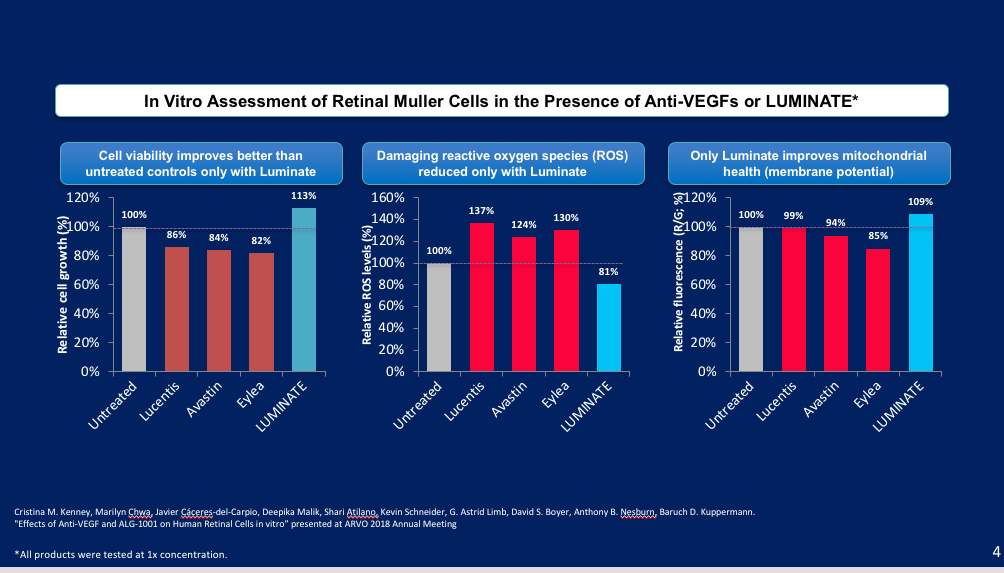
(Figure 4) In this in vitro assessment using retinal Muller cells, anti-VEGF therapies increased oxidative stress, while the anti-integrin therapy (Luminate) was shown to be neuroprotective. (Figure courtesy of Allegro)
Glenn Jaffe, MD, and his team at Duke recently treated cultured human retinal pigment epithelial (RPE) cells with hydroxyquinone in the presence or absence of the anti-integrin therapy. In these experiments, they found that cell injury and reactive oxygen species (ROS) production was reduced in the treated RPE cells.
Baruch Kuppermann, MD, PhD, Cristina Kenney, MD, PhD, and other researchers at UC-Irvine investigated the impact of several anti-VEGF and anti-integrin therapies on retinal Muller cells to evaluate whether the treatments were neuroprotective. They found that only the anti-integrin-treated groups (not any of the anti-VEGF-treated groups) had increased cell viability, reduced reactive oxygen species damage, and improved mitochondrial health (Figure 4).2
Studies like these help to make sense of the clinical results showing that anti-integrin therapy is most effective in those who are poor- or non-responders to anti-VEGF therapy, and less effective in treatment-naïve patients. The latter may simply be at a more VEGF-driven stage of the disease, while other oxidative stress pathways are implicated among those who have already undergone and failed treatment.
These findings need to be confirmed in phase III trials, but the basic science provides some optimism that this class of drugs may help patients who have been unsuccessful with other therapies.
For many years ophthalmologists have thought of DME as primarily a VEGF-mediated condition. Ophthalmologists are now discovering that multifactorial pathways-all related to oxidative stress-may play a much greater role than originally thought.
Future studies will continue to elucidate this role, and it is hoped they will provide the information ophthalmologists need to best target therapies to achieve improved visual outcomes for more DME patients.
Disclosures:
David S. Boyer, MD
P: 213/483-8810 or E: vitdoc@aol.com
Dr. Boyer is co-founder of Retina Vitreous Associates Medical Group, with six offices in and around Los Angeles. He is a consultant and member of Allegro's Scientific Advisory Board and has stock options in the company. He also serves as a consultant to Allergan, Bayer, Genentech, Regeneron, and Roche.
References:
1. Dugel PU, Layton A, Varma R. Diabetic macular edema diagnosis and treatment in the real world: An analysis of Medicare claims data (2008 to 2010). Ophthalmic Surg Lasers Imaging Retina 2016;47:258-267.
2. Kenney CM, Chwa M, Cáceres-del-Carpio J, et al. Effects of anti-VEGF and ALG-1001 on human retinal cells in vitro. Association for Research and Vision in Ophthalmology Annual Meeting, 2018.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.