AAO 2023: Post-hoc analysis of the YOSEMITE and RHINE clinical trials
Marco A. Zarbin, MD, spoke with the Ophthalmology Times team about conducting a post-hoc analysis of the YOSEMITE and RHINE clinical trials and presenting the results at this year's American Academy of Ophthalmology meeting.
Marco A. Zarbin, MD, spoke with the Ophthalmology Times team about conducting a post-hoc analysis of the YOSEMITE and RHINE clinical trials and presenting the results at this year's American Academy of Ophthalmology meeting.
Video Transcript
Editor's note - This transcript has been edited for clarity.
David Hutton:
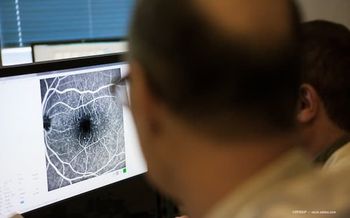
I'm David Hutton of Ophthalmology Times. The American Academy of Ophthalmology held its annual meeting recently in San Francisco. I'm joined today by Dr. Marco A. Zarbin. At the recent Academy meeting, he presented a poster titled, "Clinical Outcomes of Diabetic Macular Edema Patients Treated with Faricimab and Aflibercept: A sub cohort analysis of 20/50 or worse visual acuity across faricimab phase 3 clinical trials." Thank you so much for joining us today. Tell us about your presentation.
Marco A. Zarbin, MD:
Well, thank you very much for asking me to speak with you today. We conducted a post-hoc analysis of the YOSEMITE and RHINE clinical trials that compared faricimab, which is a combined angiopoietin-2 VEGF-A inhibitor with aflibercept in the treatment of patients with center-involving diabetic macular edema. Now, the reason we did the analysis is that a few years ago, there was a study called PROTOCOL-T, which compared the ability of aflibercept, ranibizumab, and bevacizumab to treat patients with center-involving diabetic macular edema. The patients were randomly assigned to receive 1 of those 3 drugs, and one of the important findings of PROTOCOL-T was that, in the first year of the study, the patients who had entry level visual acuity of 20/50, or worse on the etdrs chart, had a better visual outcome with aflibercept than one with ranibizumab or bevacizumab. And we wondered if there would still be a superiority of aflibercept with this new agent, called faricimab. What we found, in short, is that the visual outcome among this special group of patients is the same with faricimab is with aflibercept. But we found that the faricimab was a much better drying agent. It created a central subfield thickness less than 280 microns much more quickly, and with fewer injections, than what with aflibercept, 20 to 24 weeks versus 42 weeks. Comparing faricimab to aflibercept and in addition, it created a total absence of interactional fluid much more quickly, with faricimab than with aflibercept with the absence being present between weeks 44 and 48 with the faricimab cohorts, and week 92 with the aflibercept cohort, and that's, in other words, dry retina 10 months earlier and with fewer injections, with the faricimab 6 milligrams versus the aflibercept 2 milligrams. And finally, the durability we found was quite good. With about 76% of the patients being maintained with their injections every 12 to 16 weeks.
David Hutton:
What's the next step for this research?
Marco A. Zarbin, MD:
Well, of course, this is a post hoc analysis. And ideally, we could repeat this using a prospective analysis. And I suspect that that won't be done in the context of a pharmaceutical company sponsored study. But I think it'll probably be done by people in practice groups of people in practice. I also think that we will probably end up comparing aflibercept versus faricimab according to a treat and extend protocol. Now, in fact, in YOSEMITE and RHINE faricimab was applied using a treat and extend protocol, but the aflibercept was not. I happen to think that because the aflibercept was used at the absolute highest frequency possible, which is to say 4 monthly loading- 5 monthly loading doses and then every 8 weeks thereafter, it seems to me unlikely that a treat and extend protocol with aflibercept is going to give a result that's significantly different from what we observed in the post-hoc analysis. I'm a paid consultant for Genentech Roche, who manufactures and distributes faricimab.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.