APL-2 slows growth of GA in phase II safety and efficacy trial
Twelve-month results of the FILLY trial show that in patients with geographic atrophy, the administration of complement C3 inhibitor APL-2 slowed the growth rate of the disease. It also appeared to increase the risk of new onset AMD, although this did not have an adverse effect on visual outcomes.
By Steve Lenier; Reviewed by David Boyer, MD
Twelve-month results of the phase II FILLY trial showed that the administration of APL-2, a complement C3 inhibitor (Apellis Pharmaceuticals), slowed the growth rate of geographic atrophy (GA) in patients.
Researchers also found that while APL-2 slowed the growth rate of GA–independent of any genetic biomarkers–it also appeared to increase the risk of new onset age-related macular degeneration (AMD), although this did not have an adverse effect on visual outcomes. There also were no safety issues that would preclude further development.
In presenting the results, David Boyer, MD, Retina-Vitreous Associates Medical Group, Los Angeles, said it is well known that the complement C3 inhibitor plays a role in the development of AMD.
Dr. Boyer explained that C3 plays a central role in the complement cascade. When C3 is inhibited, as was done in this study with APL-2, all 3 activation pathways of complement are blocked, and prevents cleavage into C3a and C3b. This also prevents the downstream effects of complement, including formation of the membrane attack complex (MAC).
Study endpoints
The primary efficacy endpoint in the study was mean change in square root GA area from baseline to month 12. Two key secondary endpoints were also studied–change in best corrected visual acuity (BCVA) and the incidence of new onset AMD.
APL-2 was administered monthly in about 80 patients, and every other month in about 80 patients. For the sham groups, there were about 40 patients in the monthly group and 40 in the every-other month group.
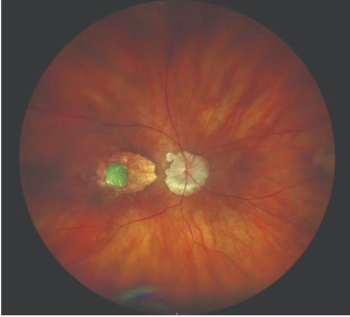
A central reading center confirmed eligibility and the size of the GA lesion in all patients, using fundus autofluorescence. The total geographic area was 2.5 mm2 to 17.5 mm2, or 1 to 7 disc areas at screening.
BCVA was 24 ETDRS letters or better, about 20/320 Snellen equivalent. There was no exclusion for fellow eye disease.
Baseline characteristics were similar for all the groups. They were well balanced as to age, gender and race. The incidence of bilateral GA was extremely high, ranging from about 85% to 90%.
History of choroidal neovascularization (CNV) in the fellow eye, however, was higher in the APL-2 monthly group. The GA areas in mm2 were smaller for the APL-2 monthly group, but well matched otherwise.
Study results
The 12-month results for mean change in square root GA lesion size showed that, compared to the sham group, there was a 28.6% reduction in the patients receiving APL-2 monthly and about 20% reduction in the patients on every-other month dosing. These treatment effects were independent of any genetic biomarkers, and were statistically significant at the pre-specified 0.1 level.
The effect increased in the second 6 months of treatment, during which monthly and every-other month APL-2 slowed GA growth by 47% (p < 0.001) and 33% (p = 0.01) respectively vs sham.
There were no differences observed in visual outcomes between the groups. This was measured to see if there was any toxicity, or any worsening, with the administration of drug. The study was not powered to determine differences in vision.
There was new onset of wet AMD present overall in the groups. In the sham group, 1% of patients developed wet AMD. In the group receiving APL-2 every other month, it was 8%, and in the monthly group, it was 18%.
“If you subdivide those into the patients who had no history or presence of CNV in the fellow eye, you can see that it was only about 10% in the monthly group and 4% in the every-other month group, and, 2% in patients who received sham,” Dr. Boyer said. “However, if the other eye had a history of CNV, the rate of conversion to wet AMD was 29% in the group receiving the APL-2 drug on a monthly basis.”
Adverse events were similar between the groups, mostly related to conversion to wet AMD. There were 2 cases of endophthalmitis in the monthly group, and 1 in the every0-other month group. Two were coagulase-negative Staphylococcus, and the other was a sterile inflammation.
David Boyer, MD
This article was adapted from a presentation that Dr. Boyer delivered at the Retina Subspecialty Day help prior to the 2017 American Academy of Ophthalmology meeting. Dr. Boyer is a consultant for Apellis.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.












































