Considering body posture after macular hole surgery
Retina surgeons discuss the need for face-down positioning after macular hole surgery. The interpretation of what constitutes “face-down” is key to their messages.
It is the responsibility of surgeons to provide patients the opportunity for their best chance at success, and with that in mind, retina surgeons should know that while macular hole surgery can be effective without face-down positioning, the highest success rates are achieved with some form of face-down positioning, said John S. Pollack, MD.
Recent:
“Patients can be counseled that face-down positioning does not require lying in the prone position, but only that the head be tilted forward so that the eyes are looking down, such as in a position used for reading or texting,” said Dr. Pollack, assistant professor of ophthalmology, Rush University Medical Center, Chicago. “Armed with all of this information, individuals can then decide for themselves whether face-down positioning is worth the effort.”
Ehab N. El Rayes, MD, PhD, offered a somewhat different perspective on the issue of face-down positioning after macular hole surgery that is based on his review of outcomes data, knowledge about mechanisms of macular hole closure and healing, and the aim of obtaining patient consent for surgery and increasing postoperative comfort.
Recent:
However, he still advises patients about postoperative positioning, telling them to avoid lying supine on their backs, but that it is okay to sit or sleep on their side.
Dr. El Rayes said that vitrectomy with internal limiting membrane (ILM) peeling and 95% gas fill provides the conditions needed for success-these techniques increase retinal elasticity, keep the edges of the hole dry for at least 7 days without supine positioning, and trigger and support the process of retinal healing. Phacoemulsification is also performed to avoid cataractous changes and maintain optical clarity.
Sponsored:
“Then, surgeons speaking to elderly patients are more likely to encourage their acceptance of the macular hole procedure by saying, ‘For 1 week, you should stay sitting or sleep on your side opposite to the side of your surgery, but not on your back’ than to say, ‘You have to stay strictly in a face-down position’,” said Dr. El Rayes, professor of ophthalmology, retina department Institute of Ophthalmology, Cairo, Egypt.
Other literature on the subject
Looking at the world’s literature, Dr. El Rayes identified 21 articles published in major peer review journals reporting on 867 eyes that underwent macular hole surgery without face-down positioning. The primary success rate in those papers ranged from 79% to 98%, and was at least 90% for hole closure without a face-down position in 16 of the 21 reports that included a total of 763 eyes.
Taking a more critical look at the literature, Dr. Pollack said that after excluding posters, articles appearing in online only journals, and studies with fewer than 50 subjects, only four studies on macular hole surgery without face-down positioning remain. However, the data are credible in only two of the four studies, and they represent the two studies that report the lowest closure rates, 81% and 87%, respectively.
Related:
One of the two remaining studies reported a 96% closure rate. However, the authors also note that 20% of patients used face-down positioning for at least 30 hours.
In the fourth study, which was designed as a retrospective review of 102 consecutive cases, only 70% of the eyes were included in the final analysis, which raises concern about selection bias, Dr. Pollack said.
More retina:
He noted, “The best paper of the four was a prospective multicenter trial that included ILM peeling with dye, gas selection based on hole size, and randomized patients to face-down or no positioning. In that study, the closure rate was 87% for the 72 eyes in the no positioning group and 97.4% for the 78 eyes assigned to face-down positioning.”
Including the latter study, Dr. Pollack identified a total of eight papers on outcomes of macular hole surgery with face-down positioning (including supine or reading position) that met the criteria of having at least 50 subjects and not being reported either as a poster or in an online only journal. Across those eight studies, the closure rate was consistently above 90%, and it ranged from 97.4% to 100% in four of the studies.
Recent:
Pooling the data from these “credible” studies, Dr. Pollack said that the average closure rate was 95% for surgeries with face-down positioning and only 83% for no positioning.
“It is no surprise, therefore, that in the 2015 American Society of Retina Surgeons Preference and Trends Membership Survey, 94% of the 815 respondents said they recommend face-down positioning after macular hole repair,” he said.
Macular hole healing
Dr. El Rayes noted that in the 25+ years since macular hole surgery was first performed, the technique has been refined and its outcomes have improved thanks to advances in instrumentation, visualization, and imaging.
Recent:
The advances have also contributed to better understanding of the mechanisms of macular hole closure that provides a foundation for understanding why strict face-down positioning is not necessary.
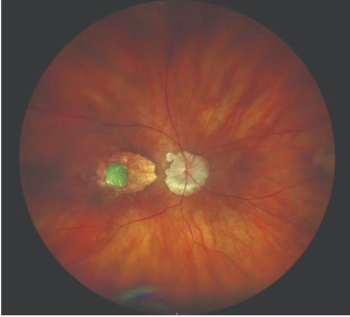
He explained that hole closure requires increasing retinal elasticity and eliminating all forms of surface traction, which is accomplished through posterior vitreous detachment and ILM peeling.
In addition, retinal detergence is necessary and is created by injecting a gas bubble. Thereafter, the tissue repair process begins, and according to several published articles, healing can happen within 1 to 2 days, Dr. El Rayes said.
Related:
“With intraoperative OCT we can see how efficiently we removed epiretinal traction and even begin to see the hole edges begin to flatten while the patient is still on the table,” he said. “Postoperatively, OCT studies have shown retinal changes such as healing, flattening, resorption of cystic fluid, and approximation of the hole edges and closure within 1 to 2 days after surgery.”
In addition, measurements of postsurgical intraocular cytokines show they are at their highest levels on day 1 after surgery, and that seems to correspond to hole closure and the reparative process, he said.
Theory on mechanisms of surgical repair
Citing a theory on mechanisms of surgical repair of macular hole developed by Mark Blumenkranz, MD, Dr. El Rayes said that removal of vitreous releases traction and allows apposition of a foreign non-porous surface (i.e., gas bubble or silicone) to the edges of the macular hole. Membrane peeling or ILM removal stimulates an intrinsic retinal wound healing response through gene activation, and these events in concert stimulate the migration of Mueller cells and associated retinal neurons that fill in the defect.
More:
Then, intrinsic photoreceptor paracrine and autocrine stimuli result in photoreceptor realignment and synapse repair, resulting in restoration of normal or near normal macular anatomy and function.
After complete fluid/gas exchange, the gas bubble serves to isolate the retina from vitreous fluid for the 5 to 7 days that it takes for macular scab contraction to occur.
Related:
Dr. El Rayes explained that based on the Pascal principle of transmission of fluid pressure, the gas bubble transmits pressure equally in all directions and creates the necessary conditions to keep the hole edges dry.
“The idea of needing first week face down positioning is inconsistent with this principle,” Dr. El Rayes said. “The gases used have a long enough half-life to isolate the macula from the vitreous in all body positions except face-up supine.”
John S. Pollack, MD
Ehab N. El Rayes, MD, PhD
This article was adapted from presentations given by Dr. Pollack and Dr. El Rayes during Retina Subspecialty Day at the 2015 meeting of the American Academy of Ophthalmology. Dr. Pollack and Dr. El Rayes have no relevant financial interests to disclose.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.