David Huang, MD, PhD, receives Lasker Award for transformative imaging technology
The Lasker-DeBakey Clinical Medical Research Award, dubbed "America’s Nobel," recognizes the wide use of optical coherence tomography to manage eye disease, prevent blindness.
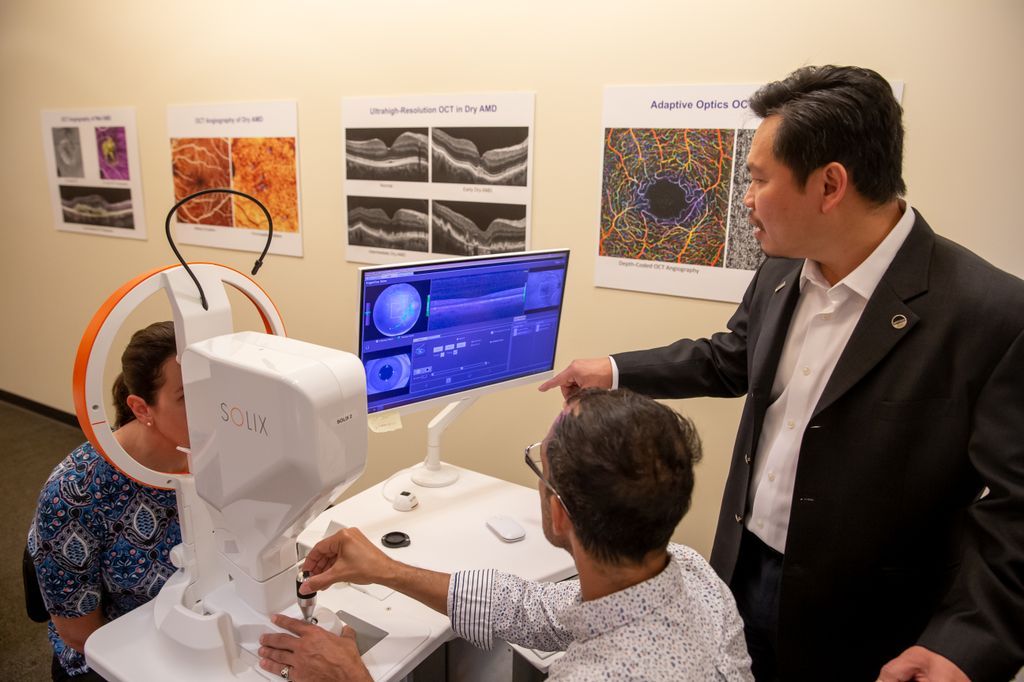
David Huang, MD, PhD, right, demonstrates a structural eye scan with the biomedical imaging technology he co-invented, optical coherence tomography, or OCT, at Oregon Health & Science University in Portland, Oregon. (Image courtesy of OHSU)
David Huang, MD, PhD, a physician-scientist at Oregon Health & Science University, is a 2023 recipient of the Lasker-DeBakey Clinical Medical Research Award for co-inventing an imaging technology that routinely helps prevent blindness and is increasingly used to diagnose and treat conditions of the heart, brain, skin and more.
The Albert and Mary Lasker Foundation recently announced the awards.
“It’s a great honor to receive the Lasker-DeBakey Award with my fellow OCT co-inventors,” Huang, director of research and associate director of the OHSU Casey Eye Institute, and professor of ophthalmology and biomedical engineering in the OHSU School of Medicine, said in a OHSU news release. “OCT may not be as well-known as other major imaging modalities, such as MRI or CT scans, but if you have a serious eye condition, chances are that you received an OCT scan to help diagnose and manage your condition. I am proud that millions of people have benefited from a technology that I helped invent three decades ago.”
According to the release, the award is one of three that the Lasker Foundation gives annually to recognize leaders who have made major advances in the understanding, diagnosis, treatment, cure and prevention of human disease. Lasker prizes are sometimes referred to as “America’s Nobels,” as 95 Lasker award winners have gone on to receive the Nobel Prize.
Huang shares this year’s Lasker-DeBakey award with fellow OCT co-inventors James G Fujimoto, PhD, and Eric A. Swanson, M, both of the Massachusetts Institute of Technology. They will be formally recognized at a Sept 29 gala ceremony in New York City.
Standard for eye disease care
The university noted in its news release OCT is used in more than 30 million imaging procedures worldwide each year to diagnose and treat the leading causes of blindness, including macular degeneration, diabetic retinopathy and glaucoma. In addition to the eye, OCT is used for medical conditions involving the heart, brain, skin, digestive tract and more. Cardiovascular specialists increasingly use it to evaluate plaque buildup and guide stent placement inside blocked arteries. OCT also helps diagnose skin cancer and measure neurodegeneration from multiple sclerosis and other neurologic conditions.
OCT has transformed the way eye disease is diagnosed and managed. The technology enables ophthalmologists and optometrists to identify vision-threatening disease early, often before patients experience symptoms.
Huang noted that during his ophthalmology residency, it was common for patients to be diagnosed with age-related macular degeneration after the disease had already progressed to the point that the loss of sight was inevitable.
“But now, OCT scans allow us to catch disease earlier and help us manage treatment so that functional vision can be maintained,” he said in the news release. This imaging technology has enabled a dramatic improvement in patient outcomes during my ophthalmology career.”
Of the nearly 20 million Americans who had age-related macular degeneration in 2019, the US Centers for Disease Control estimates fewer than 1% had developed a case that was severe enough to threaten vision.
Many people who either have or are at risk for a variety of eye diseases routinely undergo OCT scans. Each scan typically takes a few minutes and involves sitting in front of an OCT machine that sweeps an invisible beam of infrared light across the eye. OCT scans provide detailed, 3D views of structures inside the eye. An extension of the technology is called OCT angiography, which can map flow in tiny blood vessels inside the eye as well as detect the flow loss or the growth of abnormal blood vessels that are associated with many eye diseases.
Moreover, OHSU noted in its news release regular OCT scans provide detailed information about how or if disease is progressing. The university point out that the vital information drives treatment, and
This key information guides treatment. As reported in a 2017 study by Huang and colleagues, OCT saved Medicare a combined $11.2 billion between 2008 and 2015 by helping physicians decide when to provide injections for wet macular degeneration, which often leads to fewer injections.1
The origins of OCT
With an early interest in engineering, Huang worked in Fujimoto’s laser lab at MIT as an MD/PhD student. Through his work there, Huang was the first author on a key Science paper that introduced OCT in 1991, when he was 27 years old, which has since been cited in nearly 18,000 scientific publications.2
The university notes in its release the early development of OCT stemmed from Fujimoto’s interest in ultrafast lasers that generate extremely short pulses of light. Looking for a practical application for these lasers, Fujimoto asked Huang to explore using them for eye surgery and measuring the thickness of eye structures.
Fujimoto asked Swanson, who led the optical communications technology group at the MIT Lincoln Laboratory at the time, to participate. The men then developed the first OCT system, which scanned a beam of light across tissue structures to develop an image that was able to measure the beam’s reflected light wave with micrometer precision. The trio showed that OCT images could reveal microscopic structures inside the retina and the coronary artery. Their decision to test the new technology on the eye and heart proved to be prophetic: The most important uses of OCT later became ophthalmology and cardiology.
Today, Huang builds upon the development with improvements to OCT in his work at the Center for Ophthalmic Optics and Lasers at OHSU, where he leads 30 scientists, students and staff in advancing biomedical imaging. One experimental approach they’re exploring is OCT optoretinography, which measures how light-sensitive cells in the retina respond to a flash of light. Huang also partners with physicians from a variety of specialties to develop and evaluate OCT for other clinical applications.
Huang has bachelor’s and master’s degrees in electrical engineering from MIT, and a combined MD/PhD degree from the Harvard-MIT Program in Health Sciences and Technology. He completed ophthalmology residency training at the University of Southern California and cornea fellowship training at Emory University. Huang joined OHSU in 2010. As an ophthalmologist, Huang specializes in corneal diseases and refractive surgery.
The university noted in its news release that Huang holds 42 patents and has published more than 300 peer-reviewed scientific articles, He is a fellow of several professional organizations, including the American Academy of Inventors and the Association for Research in Vision and Ophthalmology. He has also been honored with an António Champalimaud Vision Award, a Visionary Prize from the Sanford and Susan Greenberg Prize to End Blindness and a Fritz J. and Dolores H. Russ Prize.
Reference:
David Huang, Kevin D. Frick, Philip J. Rosenfeld, Eric A. Swanson, Matthew A. Windsor, Sissi J.J. Sun. Study of Optical Coherence Tomography in Managing Antiangiogenic Therapy. American Journal of Ophthalmology. Published December 6, 2007. Accessed September 25, 2023. DOI: https://doi.org/10.1016/j.ajo.2017.09.027.
Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W, Hee MR, Flotte T, Gregory K, Puliafito CA, et al. Optical coherence tomography. Science. 1991 Nov 22;254(5035):1178-81. DOI: 10.1126/science.1957169. PMID: 1957169; PMCID: PMC4638169.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.