Defining terms, origins of type 3 NV
By Lynda Charters; Reviewed by K. Bailey Freund, MD
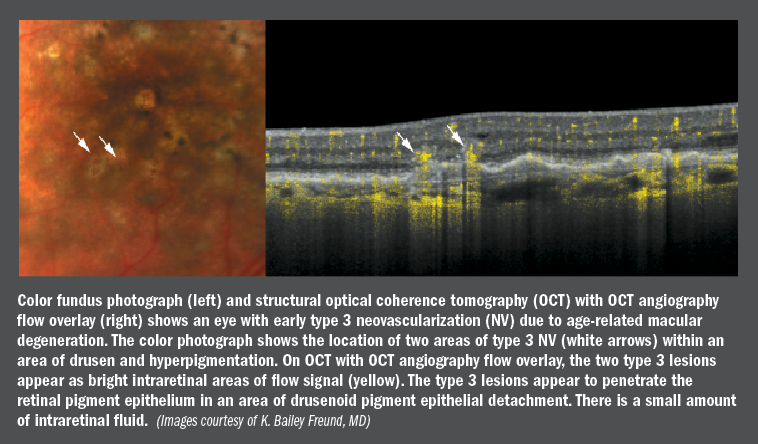
expanding on the knowledge regarding type 3 neovascularization (NV) in age-related macular degeneration (AMD) has been a painstaking process since the first report published on the presence of the lesion by Mary Elizabeth Hartnett, MD, and colleagues in the early 1990s.
According to K. Bailey Freund, MD, type 3 NV is a term that describes NV within the retina-i.e., the location, but not the origin of the pathology, and is the next logical step in the anatomic classification of NV established by J. Donald M. Gass, MD.
That classification described subretinal pigment epithelium (RPE) NV as type 1 NV and subretinal NV as type 2 NV, explained Dr. Freund, clinical professor of ophthalmology, New York University School of Medicine, New York.
Attention on type 3 NV
The origin of the lesion has received much attention since it was first recognized when Hartnett et al. suggested that the lesion be called retinal vascular abnormalities associated with pigment epithelial detachment.
Lawrence Yannuzzi, MD, and associates first proposed that type 3 NV be described by the term retinal angiomatous proliferation (RAP) in 2001, and they subclassified it into three stages as a result of imaging findings that seemed to show its origins in the retinal circulation and later was associated with the development of chorioretinal anastomosis.
Gass et al. went a step further and hypothesized that type 3 NV originated from preclinical type 1 NV forming an occult chorioretinal anastomosis.
The findings from spectral-domain optical coherence tomography (SD-OCT), real-time angiography, and OCT angiography appear to show that type 3 NV originates from the deep retinal circulation, with the latest classification based on OCT findings presuming the origin of type 3 NV to be from the deep vascular complex followed by a disruption of outer retinal layers and penetration through the RPE.
In some eyes, type 1 lesions develop a type 3 component and other cases in which type 3 lesions originate over areas of pre-existing type 1 NV. These lesions would be best classified as mixed type 1 and 3 NV, he noted.
So, this begs the question regarding why so much attention is focused on type 3 NV.
“Type 3 NV occurs almost exclusively in AMD and is far more common than previously recognized,” Dr. Freund said. “In a consecutive series of newly diagnosed treatment-naïve AMD eyes, Jung et al. identified type 3 NV as the predominant lesion component in 34.2% of their cases.”
When recognized early, type 3 NV responds well to intravitreal anti-vascular endothelial growth factor (VEGF) therapy, but over the long term, visual outcomes can be poor since these eyes are at high risk for bilateral involvement and macular atrophy.
The origin of type 3 NV still is unclear. However, researchers who evaluated submacular tissue obtained intraoperatively and intact post-mortem eyes have pointed to retinal and not choroidal sources because of the absence of vascular connections through defects in Bruch’s membrane.
Case study
To shed more light on the genesis of type 3 NV, Dr. Freund and colleagues attempted to correlate in vivo OCT findings with post-mortem histologic findings in a patient with AMD who was treated with anti-VEGF therapy.
In this case, an 86-year-old Caucasian woman had type 3 NV secondary to AMD in her right eye that was treated with six intravitreal injections of bevacizumab (Avastin, Genentech). Geographic atrophy was present in the left eye and reticular pseudodrusen were present bilaterally.
At the initial visit, visual acuity in the right eye with type 3 NV was 20/80. OCT was performed each month out to 6 months and included serial near-infrared reflectance and eye-tracked SD-OCT. This retinal imaging was correlated with ex vivo and high-resolution histologic images of the preserved donor eye evaluated at month 10. Clinical improvement was apparent in the images over time.
The main outcome measures included reflectivity of the vascular complex, intraretinal hyperreflective foci and intraretinal cellularity, analysis of the topography of pathologic features, and evaluation of the sub-RPE and the basal lamina (BL) space.

Dr. Freund reported that “the clinical imaging showed a deep neovascular lesion in close relationship with a mixed serous and drusenoid pigment epithelium detachment (PED) characteristic of type 3 NV. Antiangiogenic therapy achieved complete resolution of the exudation. The PED progressively flattened with each treatment, leaving a persistent triangular hyperreflectivity in the outer retina, which was correlated histologically with a vascular complex implanted into sub-RPE basal laminar deposit (BLamD). No connection between the choriocapillaris and the sub-RPE plus BLamD space was observed. Both the RPE-derived and lipid-filled cells were correlated with clinical intraretinal hyperreflective foci. The sub-RPE plus BLamD space contained macrophages, lymphocytes, Müller cell processes, and subducted RPE.”
The authors published their findings (Ophthalmology. 2018;125:276-287. doi: 10.1016/j.ophtha.2017.08.019. Epub 2017 Sep 28).
This case study showed the clinicopathologic correlation of type 3 NV with vascular elements of retinal origin accompanied by collagenous material and Müller cell processes implanted into the thick sub-RPE basal laminar deposit, which may simulate the appearance of chorioretinal anastomosis. Surrounding RPE-derived and lipid-filled cells, possibly microglia, were correlated with clinical intraretinal hyperreflective foci.
“In this patient with type 3 NV, there was no evidence of a choroidal origin of the lesion,” Dr. Freund concluded.
K. Bailey Freund, MD
e: kbfnyf@aol.com
Dr. Freund is a consultant to Genentech, Heidelberg Engineering, Optos, and Optovue, and has received research support from Genentech.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.