Early intervention best for patients with diabetic eye diseases
When it comes to diabetic eye diseases, there are a multitude of potential treatments-but perhaps the “easiest” one for patients is to ensure their A1C levels are under control.
When it comes to diabetic eye diseases, there are a multitude of potential treatments-but perhaps the “easiest” one for patients is to ensure their A1C levels are under control.1
For those with type 1 diabetes, fasting glucose levels may be as much as 3 times the normal range (70-100 mg/dL), whereas those with type 2 diabetes often have high-fasting glucose levels of 150 mg/dL or higher.
According to Versant Health, diabetes affects more than 30 million Americans (about 9.4% of the population). Of those, nearly 30% (or 10 million people), have diabetic retinopathy (DR), a potentially blinding disease that costs Americans more than $500 million every year.
In its white paper, "The health and financial costs of diabetic retinopathy," Mark Ruchman, MD, Chief Medical Officer at Versant Health and Elizabeth Klunk, RN, senior vice president of Versant Health, note that 20% of people first learn they are diabetic through the results of an eye exam.
According to the American Academy of Ophthalmology (AAO),1 15 years after diagnosis, 80% of those with type 1 will have developed DR (whereas only 25% are likely to have developed DR after 5 years). Those with type 2 tend to fare worse-as 84% of those taking insulin are likely to have DR 19 years after diagnosis, and proliferative DR is likely in 25% of patients with type 2 diabetes’ duration of 25 years or more.
“Early intervention is critical when it comes to the successful treatment of diabetic retinopathy,” Dr. Ruchman said. “In its early stages, when treatment has the greatest likelihood of success, patients are typically asymptomatic. Thus, a regular eye exam is a critical component of any health and wellness program to reduce blindness from this disease.”
Patients with diabetes face numerous health risks, including glaucoma, cataracts, and diabetic macular edema (DME) or DR. Beyond just diabetes, inflammation and obesity increase the risk of developing DR, the white paper reports.
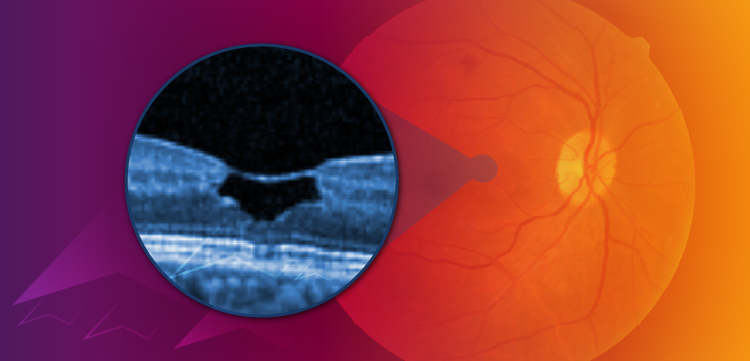
Damage to the ocular system progresses through four phases-first, microaneurysms develop which then become progressively blocked.
That, in turn, results in the retina being denied the nourishment it needs, which results in sending signals to grow more blood vessels. Those blood vessels are more fragile and when they leak patients respond by noticing blurred vision, vision loss, and (eventually if left untreated) blindness.
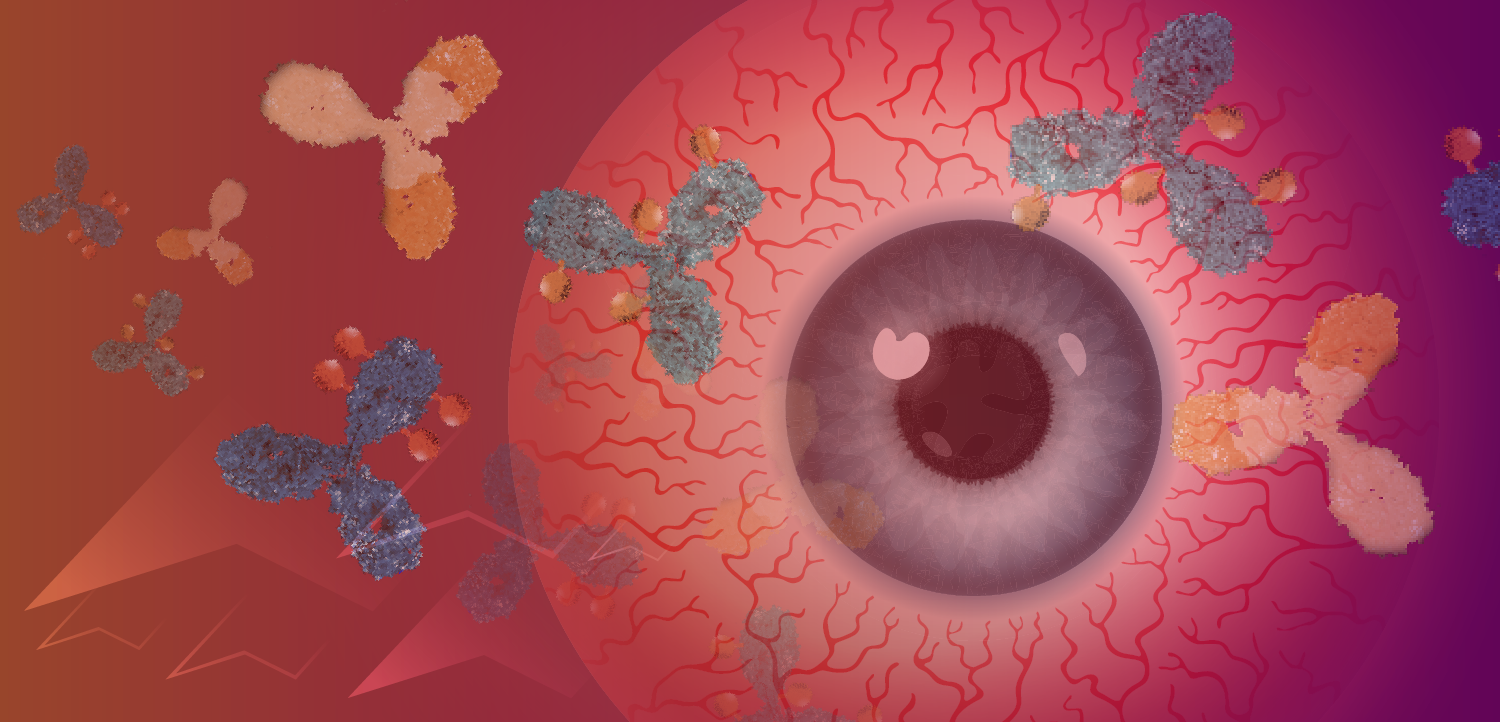
People with uncontrolled blood pressure also show these signs and symptoms, but treatment for this condition (hypertensive retinopathy) should be treated with laser, with intravitreal corticosteroids, or by the anti-vascular endothelial growth factor (VEGF) agents.
The white paper also cites the National Institute of Diabetes and Digestive Kidney Diseases’ statistics that early detection and treatment can reduce the risk of blindness from diabetes by 95%. In fact, the risk of developing DR can be reduced by 76% and the rate of progression slowed by 54% if patients undergo intensive treatment.2
Unfortunately, early in the disease state most patients are asymptomatic, meaning an annual eye exam can be of paramount importance in the detection of diabetic eye disease.
While AAO notes about 40% of people with diabetes forego an annual eye exam for DR,1 Murchison et al.3 found in an urban academic center, only 42% of patients adhered to initial follow-up eyecare recommendations. That group found the more severe the disease, the more likely people were to adhere to timely dilated fundus exams. Specifically, patients with mild and moderate DR, patients with normal vision, patients who smoke are at a greater risk for poor follow-up eye care adherence.3
Versant Health added the cost of diabetes to the United States is about $327 billion annually, with $237 billion in direct medical costs (the remainder from lost or decreased productivity). Average Medicare payments were significantly higher for patients with nonprofilerative DR and proliferative DR than for patients with diabetes but neither of those categories. Overall, patients with DR have higher medical costs than those with other types of diabetic complications.
Finally, AAO advises communicating “both ophthalmologic findings and level of retinopathy to the primary-care physician (PCP). They should emphasize to the patient the need to adhere to the PCP’s guidance to optimize metabolic control.”1
References:
1. American Academy of Ophthalmology Retina Panel. Preferred Practice Pattern: Diabetic Retinopathy. San Francisco, CA: AAO, 2016.
2. Aiello LP, Group DER. Diabetic retinopathy and other ocular findings in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. 2014;37(1):17-23.
3. Murchison AP, Hark L, Pizzi LT, et al. Non-adherence to eye care in people with diabetes. BMJ Open Diabetes Res Care. 2017;5(1):e000333.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.