FDA-approved drug demonstrates potential in lab models for blinding childhood disease
According to National Eye Institute researchers, the strategy may speed the delivery of therapeutic options relative to time it would take to develop gene therapies.
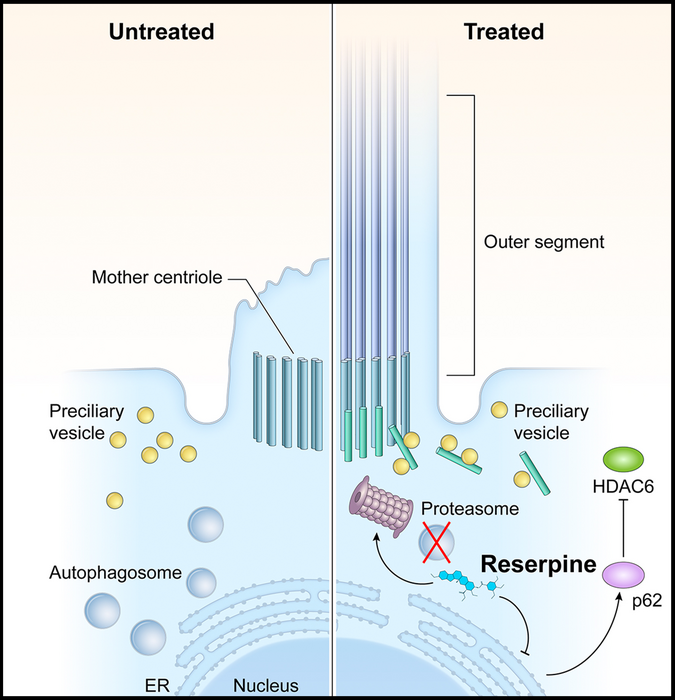
In LCA10, CEP290 mutations lead to defects in the photoreceptor outer segment. Consequently, the building blocks of the primary cilium accumulate in the photoreceptors, which activates autophagy (shown left, untreated). Reserpine restores the balance between autophagy and the ubiquitin-proteasome system histone deacetylase 6 and improves primary cilium assembly. (Image courtesy of NEI/Holly Y. Chen, PhD)
A National Eye Institute-led team has identified a compound already approved by the U.S. Food and Drug Administration that keeps light-sensitive photoreceptors alive in three models of Leber congenital amaurosis type 10 (LCA 10), an inherited retinal ciliopathy disease that often results in severe visual impairment or blindness in early childhood.
According to an NIH/NEI news release, LCA 10 is caused by mutations of the cilia-centrosomal gene (CEP290). Such mutations account for 20% to 25% of all LCA – more than any other gene.
Using a mouse model of LCA10 and two types of lab-created tissues from stem cells known as organoids, the team screened more than 6000 FDA-approved compounds to identify ones that promoted survival of photoreceptors, the types of cells that die in LCA, leading to vision loss. The high-throughput screening identified five potential drug candidates, including Reserpine, which was approved in 1955 for the treatment of high blood pressure. Improved medications for hypertension have since become available.
“Observation of the LCA models treated with Reserpine shed light on the underlying biology of retinal ciliopathies, suggesting new targets for future exploration,” said the study’s lead investigator Anand Swaroop, PhD, senior investigator and chief of the NEI Neurobiology Neurodegeneration and Repair Laboratory. The work was performed in collaboration with the National Center for Advancing Translational Sciences, both part of the National Institutes of Health.
Moreover, the NHI/NEI news release noted the models showed dysregulation of autophagy, the process by which cells break down old or abnormal proteins, which in this case resulted in abnormal primary cilia, a microtubule organelle that protrudes from the surface of most cell types. Once thought to be an evolutionary vestige, the primary cilium has emerged as a key organelle that senses the external environment and modulates signaling pathways in many types of tissue. Gene mutations that lead to primary cilium dysfunction are linked to numerous diseases, collectively called ciliopathies, which range from kidney and brain malformations to congenital retinal degeneration.
According to the release, in LCA10, CEP290 gene mutations cause dysfunction of the primary cilium in retinal cells. Reserpine appeared to partially restore autophagy, resulting in improved primary cilium assembly.
Reserpine targets dysregulated intracellular signaling pathways downstream of the primary cilium. Such a treatment strategy could potentially address retinal ciliopathies caused by many of the more than 160 disease-causing genes, regardless of the specific gene involved. That’s in contrast to gene therapy, which requires a very expensive and labor-intensive process to tailor an individual gene-based therapeutic approach for each mutation.
“Patients suffering from vision loss due to photoreceptor cell death might eventually benefit from our findings, as small molecule drugs represent a relatively affordable and scalable option,” Swaroop said in the release.
“Repurposing already FDA‐approved drugs reduces the cost and accelerates the transition from bench to bedside,” he explained.
Dose‐response and toxicity assays will be performed soon to demonstrate the safety of reserpine‐derived drugs for clinical trials.
This work was supported by the NEI Intramural Research Program (ZIAEY000450 and ZIAEY000546) and the NCATS Intramural Research Program (ZIATR000018-06).
Reference:
Chen HY, Swaroop M, Papal S, Mondal AK, Song HB, Campello L, Tawa GJ, Regent F, Shimada H, Nagashima K, de Val N, Jacobson SG, Zheng W, Swaroop A. “Reserpine maintains photoreceptor survival in retinal ciliopathy by resolving proteostasis imbalance and ciliogenesis defects,” Published online Mar 28, 2023 in eLife https://doi.org/10.7554/eLife.83205
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.