How I use MicroPulse Laser to treat DME
Dr. Jorge Calzada shares his methods for treating diabetic macular edema with MicroPulse Laser and anti-VEGF injections.
When I began treating with MicroPulse laser two years ago, I referred to information from Iridex and looked at settings used by other doctors. Then, I began to experiment and discover the settings that worked best for me.
There are a multitude of setting combinations that produce safe and effective results. A doctor’s choice is a little like their recipe for home cooking. It is what works for them based on their patient population.
With the Iridex IQ 577 Laser, I use a 5% duty cycle, for a duration of 200 milliseconds (ms). Laser energy is being delivered 5% of the time over the 200-ms duration. I usually use a flat macular contact lens for visualization, but there are multiple macular lenses that can be used reliably.
Before performing the procedure, I titrate power in the laser’s MicroPulse treatment mode, since some eyes demonstrate more laser uptake than others. I do this using a single 100-µm spot and a 200-ms duration. I start with 1000 milliwatts (mW), outside the macula, near the arcades, and continue to raise or lower the power in 50 mW increments – moving to a new area each time – until I see minimal macular whitening.
I note the power at which I observed the minimum effect during the test spot and reduce that power by half before delivering MicroPulse laser. The result is usually between 500 mW and 700 mW. I retain the 100-µm spot size, but I switch from a single spot to a three by three grid using Iridex’s TxCell Scanning Laser Delivery System that is compatible with the IQ 577 laser. I have colleagues who successfully use a larger grid, but I like the smaller grid, because I find that patients sometimes move during treatment.
With the TxCell, the distance between the spots can be adjusted within a given pattern. Due to the lack of a visible burn and limited thermal spread, MicroPulse laser treatment is performed with high-density placement of confluent applications to maximize its therapeutic effect.1 There’s a tendency for new MicroPulse users to undertreat by not placing enough spots, so the it’s worth keeping in mind the benefit of a high density treatment.
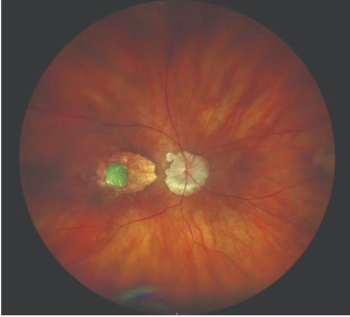
I usually treat both the area of edema visible with optical coherence tomography and the area of leakage on the intravenous fluorescein angiography. Usually these overlap, but there can be leakage outside of the edematous area.
It’s no problem to integrate MicroPulse therapy into the middle of my daily clinic routine. I have the patient sit upright in a height-adjustable chair, in a dedicated laser treatment room. During the procedure, my assistant makes sure the patient remains still.
There’s no patient preparation required aside from dilation and topical anesthesia for the contact lens, and the patient can go home immediately after the procedure.
I’ll usually bring the patient back in about six weeks. In concerning cases and those that also involve anti-VEGF injections, I’ll have them come back in four weeks.
If the MicroPulse treatment resolves the edema, I will not repeat the procedure. If the MicroPulse treatment improves the condition, but does not resolve it entirely, I may repeat it once or twice. I wait three to four months between treatments, to see the full response to treatment before retreating. If the condition is not entirely resolved after two re-treatments, I try another intervention.
In cases where the fovea is involved, I combine MicroPulse therapy with anti-VEGF injections. Edema involving the fovea usually affects vision, and the effect of anti-VEGF injections sets in faster. I don’t do injections and MicroPulse therapy at the same time, however, because I want to be able to observe the results of a specific treatment.
Reference
1. Lavinsky D, Cardillo JA, Melo LA, Jr, et al. Randomized clinical trial evaluating mETDRS versus normal or high-density MicroPulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52(7):4314-4323.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.