ICYMI: State of AMD research in 2018
The year 2018 had its share of groundbreaking research in age-related macular degeneration (AMD). Here is a brief overview of what’s been presented or published within the past 12 months.
JAMA Ophthalmology
Jennifer Abbasi, senior staff writer, JAMA Medical News, and Feyza Sancar, PhD, Editor of JAMA Medical News, evaluated all the original research published across the entire realm of the JAMA network to discuss the most-read topic in each of the journals. In ophthalmology, that was the work of the Everest II Study Group.
A randomized clinical trial compared ranibizumab with or without verteporfin photodynamic therapy (PDT) for the treatment of polypoidal choroidal vasculopathy (PCV).1 This particular type of age-related macular degeneration is common among Asian patients. (PCV is an exudative retinal disease characterized by an abnormal subretinal pigment epithelial network of vessels of choroidal origin, ending in aneurysmal dilatations. PCV can lead to chronic, multiple, recurrent serosanguineous detachments of the retinal pigment epithelium and retina.) If left untreated, the long-term visual prognosis of patients with PCV is poor.
“The researchers found that combining intravitreal ranibizumab with PDT resulted in greater visual acuity improvement compared with ranibizumab alone,” Abbasi said. The combination resulted in an improvement of 8.1 letters, compared with 5.1 letters with monotherapy treatment.
According to the study authors, after 12 months, the combination therapy “was not only noninferior but also superior to ranibizumab monotherapy… and superior in complete polyp regression while requiring fewer injections.”1
Vitreous hemorrhage was the only serious ocular adverse event.
The full list of top-read JAMA publications in 2018 (and the editors’ assessments) is available
Brolucizumab data showing promise
Anti-vascular endothelial growth factor (VEGF) agents are first-line treatments for AMD, but not all patients respond, some require monthly dosing, and even without monthly dosing, monthly evaluation is generally recommended.
Brolucizumab is a humanized single-chain antibody fragment that inhibits all isoforms of VEGF-A and is designed to be used every 12 weeks (after a traditional 3-month dose loading phase). Researchers are also evaluating an 8-week dosing option dependent upon disease activity.
HAWK and HARRIER are two phase 3 studies evaluating the compound. More than 1,800 patients across 400 centers worldwide have been enrolled, making these studies “the first and only global head-to-head trials in patients with neovascular AMD that prospectively demonstrated efficacy at week 48 using an innovative q12w/q8w regimen, with a majority of patients on q12w immediately following the loading phase,” according to Novartis.
Both studies are 96-week prospective, randomized, double-masked multi-center studies comparing the efficacy and safety of intravitreal injections of brolucizumab 6 mg (HAWK and HARRIER) and 3 mg (HAWK only) versus aflibercept 2 mg in patients with neovascular AMD.
Phase III results from year 2 that reaffirmed its positive year 1 findings, according to developer Novartis. Brolucizumab met its primary endpoint of non-inferiority versus aflibercept in best-corrected visual acuity (BCVA) and exhibited superiority in key retinal outcomes at year one (48 weeks).2
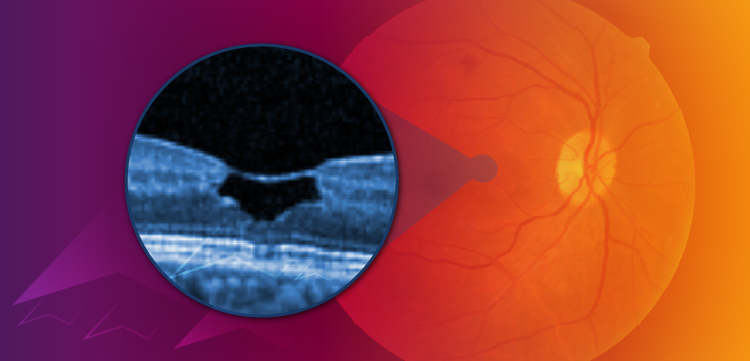
At week 16, relative to aflibercept, 35% fewer brolucizumab 6 mg patients showed presence of intraretinal fluid (IRF) and/or subretinal fluid (SRF) in HAWK, and 33% fewer in HARRIER (p < 0.0001 for both).3,4
Again at week 48, relative to aflibercept, 31% fewer patients on brolucizumab 6 mg had IRF and/or SRF in HAWK, and 41% fewer in HARRIER (p < 0.0001 for both). Brolucizumab 6 mg patients demonstrated superior reductions in central subfield thickness (CST).
Significantly improved CST reductions were evident at week 16 (p = 0.0016 in HAWK and p < 0.0001 in HARRIER) and at week 48 (p = 0.0023 and p < 0.0001, respectively).4
The year two HAWK and HARRIER findings demonstrated that fewer patients with neovascular AMD had intra-retinal fluid (IRF) and/or subretinal fluid (SRF)-key markers used by physicians to determine injection frequency in clinical practice-with brolucizumab 6 mg versus aflibercept at week 96 [24% for brolucizumab 6 mg versus 37% for aflibercept in HAWK (p = 0.0001); 24% versus 39%, respectively, in HARRIER (p < 0.0001)].
Sustained-release ranibizumab
LADDER (Long Acting DElivery of Ranibizumab; NCT02510794) is a phase II study designed to evaluate the efficacy and safety of the Port Delivery System with ranibizumab (PDS) in people with wet AMD who have previously responded to treatment with anti-VEGF therapies.5
This multicenter, randomized, interventional, active treatment-controlled study enrolled 243 participants in about 50 sites across the United States. The primary objective of LADDER was to determine the time until a patient first required a refill of the implant, assessing the efficacy and safety of three different concentrations of ranibizumab compared to monthly intravitreal injections of ranibizumab 0.5 mg.
The majority of PDS patients enrolled in the LADDER trial went six months or longer between implant of the device and the first, required refill. Vision outcomes in the high-dose PDS group were similar to monthly ranibizumab eye injections and were maintained throughout the study period.5
Later in the year, Genentech announced that, based on the data of the Phase 2 Ladder program, the pivotal Phase III Archway clinical trial and the Portal label extension study were initiated in September 2018. These studies will evaluate the efficacy and safety of the PDS 100 mg/mL concentration in patients with wet AMD at a fixed dosing interval of 24 weeks.6
For more details on the LADDER study, click
References:
1. Koh A, Lai TYY, Takahashi K, et al. Efficacy and Safety of Ranibizumab With or Without Verteporfin Photodynamic Therapy for Polypoidal Choroidal Vasculopathy: A Randomized Clinical Trial. JAMA Ophthalmol. 2017;135:1206-13.
2. Two-year data for Novartis brolucizumab reaffirm superiority versus aflibercept in reducing retinal fluid in patients with nAMD. Available at:
3. Dugel PU, Jaffe GJ, Sallstig P, et al. Brolucizumab Versus Aflibercept in Participants with Neovascular Age-Related Macular Degeneration: A Randomized Trial. Ophthalmology. 2017;124:1296-304.
4. Novartis. Novartis brolucizumab (RTH258) demonstrates superiority versus aflibercept in key secondary endpoint measures of disease activity in nAMD, a leading cause of blindness. Available at:
5. Genentech Unveils Positive Phase II Results for the Port Delivery System with Ranibizumab (PDS), the First-Ever Eye Implant to Achieve Sustained Delivery of a Biologic Medicine to Treat People With Wet Age-Related Macular Degeneration (AMD). Available at:
6. New STAIRWAY Study Data Shows Potential for Extended Durability With Faricimab in Wet Age-Related Macular Degeneration (AMD). Available at:
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.