Intra-arterial tissue plasminogen activator beneficial in treatment of central retinal artery occlusion
tPA treatment could provide benefits for patients with central retinal artery occlusion.
Reviewed by Gareth Lema, MD, PhD.

Central retinal artery occlusion (CRAO) is a vision-threatening disorder for which there is no well-established treatment. Intra-arterial tissue plasminogen activator (tPA) has the potential to fill that gap but it has to be given in time, according to Gareth Lema, MD, PhD, Senior Faculty, Icahn School of Medicine at Mount Sinai, New York.
Dr. Lema and colleagues believe that substantial loss of vision can be prevented by “timely treatment” of CRAO using intra-arterial tPA when it is administered within a window 6-12 hours at most after the onset of symptoms, as they reported previously.1
This treatment, however, does not come without challenges. Time is retina; and minutes count. Patients often do not present in time for treatment or unnecessary delays diagnosis affect the eligibility for treatment. Acute painless unilateral vision loss is not often perceived as a possible stroke, Dr. Lema pointed out. Even among doctors, only about a third of ophthalmologists refer patients for an emergent stroke evaluation.
If a patient presents to the emergency department on time, the only path to treatment is a full consult with an ophthalmologist, including a dilated exam.
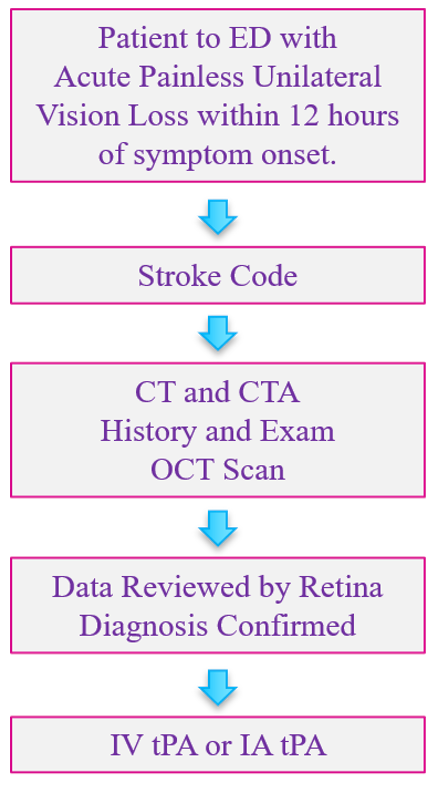
The goal of this new protocol is to remove the diagnostic delay and decrease the time to treatment to within 3 to 6 hours after symptom onset, by eliminating the onsite ophthalmology consult.
Mount Sinai experience
In the previously mentioned study, Dr. Lema recounted, visual acuity improvements were seen in 66% of the 15 patients treated with intra-arterial tPA, 53% had a 3-line improvement in vision, 4 patients who presented with counting fingers to no light perception vision improved to 20/80 vision or better. There were no major adverse events.
In the study, the mean tPA dose was 17 mg and the tPA was infused via a transfemoral arterial approach. The mean time to treatment was 8.83 hours (range, 5.5-12 hours).
Importantly, he pointed out, these improvements exceed those with the natural course of the disease and in some cases, “dramatic improvement” was achieved with earlier treatment.
Optimizing treatment
Telemedicine, which was adopted by many ophthalmologists during the COVID-19 pandemic, can be instrumental in streamlining treatment of CRAO. To expedite the diagnosis, OCT machines were placed in three stroke centers within the Mount Sinai Health System. Scans are obtained by the stroke service and transmitted to a retina attending along with history and exam data, such a visual acuity and pupil exam. The diagnosis can be made in minutes and eligible patients can rapidly obtain treatment.
Dr. Lema concluded, “CRAO is visually debilitating, but establishing collaborative relationships with our stroke colleagues and optimizing the evaluation can save vision by decreasing the time to treatment.”
Reference
Sobol EK, Sakai Y, Wheelwright D, et al. Intra-arterial tissue plasminogen activator for central retina arterial occlusion. Clin Ophthalmol 2021;15-601-8.
Related Content: Additional AAO Content | Ophthalmology | Conference Coverage
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.