Managing expectations of referring doctors and patient after retinal detachment repair
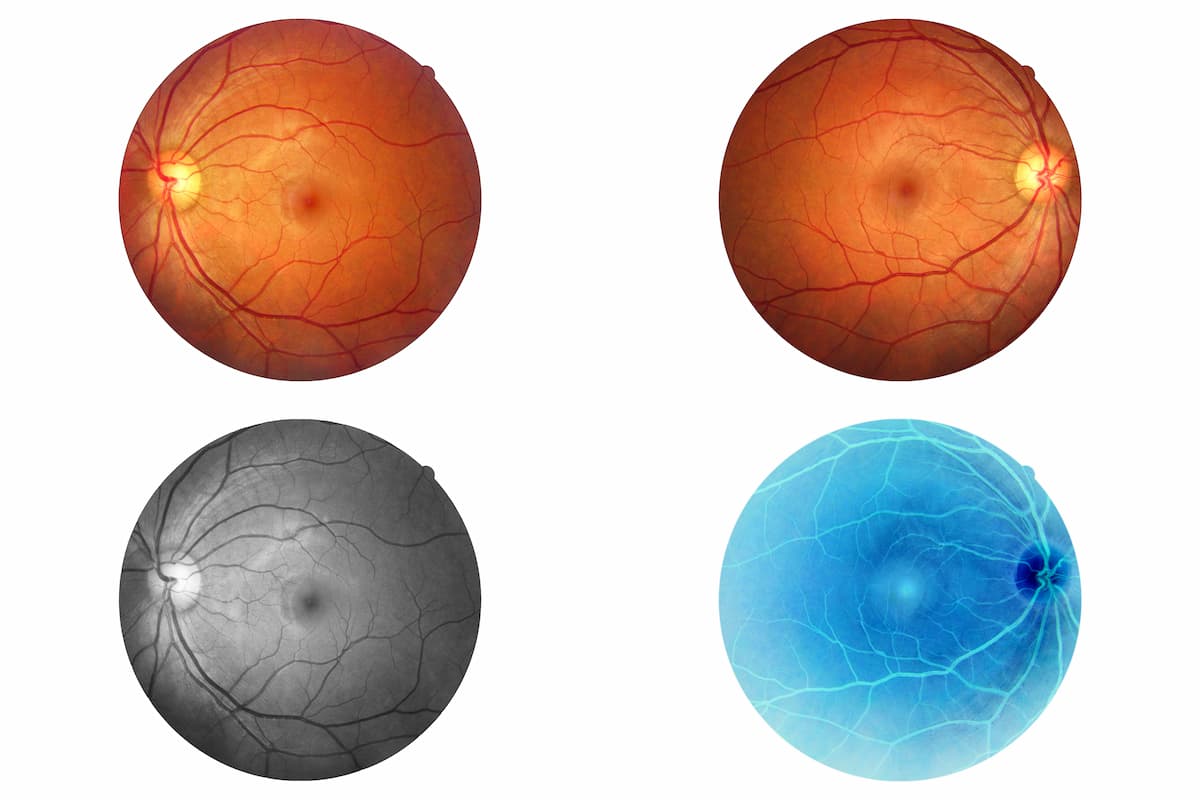
(Image credit: AdobeStock/lightmemorystock)
Reviewed by Laxmi V. Devisetty, MD
Laxmi Devisetty, MD, walked through the postoperative scenario following retinal detachment repair for referring doctors and patients at the Envision Summit 2024 in Puerto Rico. She is in private practice at Delaware Valley Retina Associates, Doylestown, PA.
For referring doctors, there are a number of factors they must consider during the management of care following retinal detachment repair. These include monitoring the intraocular pressure (IOP) in eyes filled with oil or gas tamponade, patient compliance with drop instillation, and scheduling follow-up appointments for day 1, week 1, and months 1 and 3 postoperatively.
The primary concerns for the physician may be poor intraocular view, correct maintenance of the postoperative position by the patient, monitoring of ocular pain and redness, and use of blood thinners.
Referring physicians also need to be alert to development of complications postoperatively.Specifically, these include pain, cataract development, myopia, epiretinal membranes, and development of metamorphopsia and cystoid macular edema (CME), diplopia, visual impairment, retinal re-detachment and proliferative vitreoretinal retinopathy (PVR), and the risk to the fellow eye.
“The goal for these patients,” Devisetty said, “is anatomic reattachment.”
She recounted the variations in the pooled rate of surgical complications after scleral buckling and vitrectomy for treatment of rhegmatogenous retinal detachments. The primary complications associated with scleral buckling procedures included hypotony in 23.2%, cataract in 23.6%, residual subretinal fluid in 19.6%, and postoperative PVR in 11.2%. Other much less frequent complications included iatrogenic breaks, choroidal detachment, high IOP, corneal epithelial defects, CME, macular pucker, and diplopia.
Following vitrectomy, the major complications are cataract in 53.1%, high IOP in 11.6%, and postoperative PVR in 11.1%; less frequent problems include subretinal hemorrhage, corneal epithelial defects, diplopia, CME, and macular pucker.1
Patients should be reminded of possible developments postoperatively during counseling. Importantly, they must comply with the schedule for antibiotic and anti-inflammatory drop installation and to be alert for ocular pain and redness. They should be advised of the potential for IOP increases and the need to maintain postoperative positioning in order for the tamponades to work. Their activity level should be kept to a minimum during the postoperative period. Importantly, they should be advised about the possibility of temporarily or permanently decreased vision and the risk to the fellow eye.
“It goes without saying that clinical knowledge and surgical skill are prerequisites for successful outcomes.However, it also is important to remember that effective communication with patients and referring doctors about expectations of surgery is integral in facilitating that success,” Devisetty concluded.
Reference
1. Lv Z, Li Y, Wu Y, Qu Y. Surgical complications of primary rhegmatogenous retinal detachment: A meta-analysis. PLoS ONE 2015;10:e0116493. doi: 10.1371/journal.pone.0116493.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.