Navigating Real-World Evidence in Ophthalmology
Authors: Robert P. Finger1, Taiji Sakamoto2, James Talks3, Vincent Daien4,5, Tien Wong6,7, Bora Eldem8, Paul Mitchell9, Jean-François Korobelnik10,11
1 - Department of Ophthalmology, University of Bonn, Bonn, Germany
2 - Department of Ophthalmology, Kagoshima University Graduate School of Medical and Dental Sciences, Kagoshima, and J-CREST, Japan
3 - Department of Ophthalmology, Royal Victoria Infirmary, Newcastle upon Tyne, United Kingdom
4 - Department of Ophthalmology, Gui De Chauliac Hospital, Montpellier, France
5 - The Save Sight Institute, Sydney Medical School, The University of Sydney, Sydney, NSW, Australia
6 - Singapore Eye Research Institute, Singapore National Eye Centre, Singapore, Singapore
7 - Duke-NUS Medical School, Singapore, Singapore
8 - Faculty of Medicine, Ophthalmology Department, Hacettepe University, Ankara, Turkey
9 - Centre for Vision Research, Westmead Institute for Medical Research, University of Sydney, NSW, Australia
10 - CHU Bordeaux, Service d'ophtalmologie, Bordeaux France
11 - Univ. Bordeaux, Inserm, Bordeaux Population Health Research Center, team LEHA, UMR 1219, F-33000 Bordeaux, France
Disclosures:
R. P. Finger – Consulting/paid presentations for Bayer, Novartis, Roche/Genentech, Novelion, Opthea, Inositec, Santhera, Alimera and Ellex, Research for Novartis, Zeiss and CentreVue; T. Sakamoto – Alcon, Bayer, Novartis, Santen, Senju and Wakamoto; J. S. Talks – Advisory boards for Bayer; Novartis and Allergan; Research for Bayer, Novartis, Allergan and Roche; Travel sponsorships for Bayer and Novartis; V. Daien – Alcon, Bayer, Horus, Novartis and Thea; T. Y. Wong – Abbott, Allergan, Bayer, Novartis, Pfizer and Roche; B. M. Eldem – Consultant to Bayer, Novartis, Allergan and Investigator to Roche; P. Mitchell – Consultant for Bayer, Novartis, Allergan, Roche, Abbott; J.-F. Korobelnik – Alcon, Allergan, Bayer, Beaver Visitec, Horus, Krys, Kanghong, NanoRetina, Novartis, Roche, Thea and Zeiss
The authors have no commercial interests in relation to the article. Medical writing and editorial support for preparation of the article, under the guidance of the authors, was provided by ApotheCom, which was funded by Bayer Consumer Health.
Randomised controlled trials (RCTs) are the gold standard to address clinical questions on the efficacy and safety of therapies, using strict criteria and specific methods. This stringency means that RCTs may not fully reflect treatment outcomes in routine clinical practice.1,2 Real-world data (RWD) are generated from studies that more closely represent routine clinical practice, and can include longer-term safety, effectiveness and patient-reported outcome measures. When these data are collected and analysed appropriately, the resulting real-world evidence (RWE) complements information from RCTs, providing additional information to support informed clinical decisions and enhance patient care.1-3
In the context of neovascular age-related macular degeneration (nAMD), the approval and widespread application of intravitreal anti-vascular endothelial growth factor (VEGF) agents has offered the potential to improve and stabilise patients’ visual acuity. Clinical experience from routine practice has contributed to an increased understanding of the impact of these agents on patients and their disease, and is reflected in an increasing body of RWE from a number of RWD sources.2,4 These real-world studies have provided valuable insight into long-term outcomes and utilisation of anti-VEGF agents in nAMD, but have also revealed differences in outcomes achieved with anti-VEGF agents in clinical practice, compared with RCTs.5 Identification of these disparities has allowed for variations in treatment practices to be highlighted, resulting in the opportunity to improve services, understand the need for proactive treatment and establish new treatment regimens, such as treat-and-extend.5
As with all forms of data generation, there are inherent limitations to the study designs associated with RWD collection. It is therefore important that the quality of each piece of RWE is carefully assessed, to ensure reliable conclusions can be drawn that are applicable to clinical practice.1,4,6,7
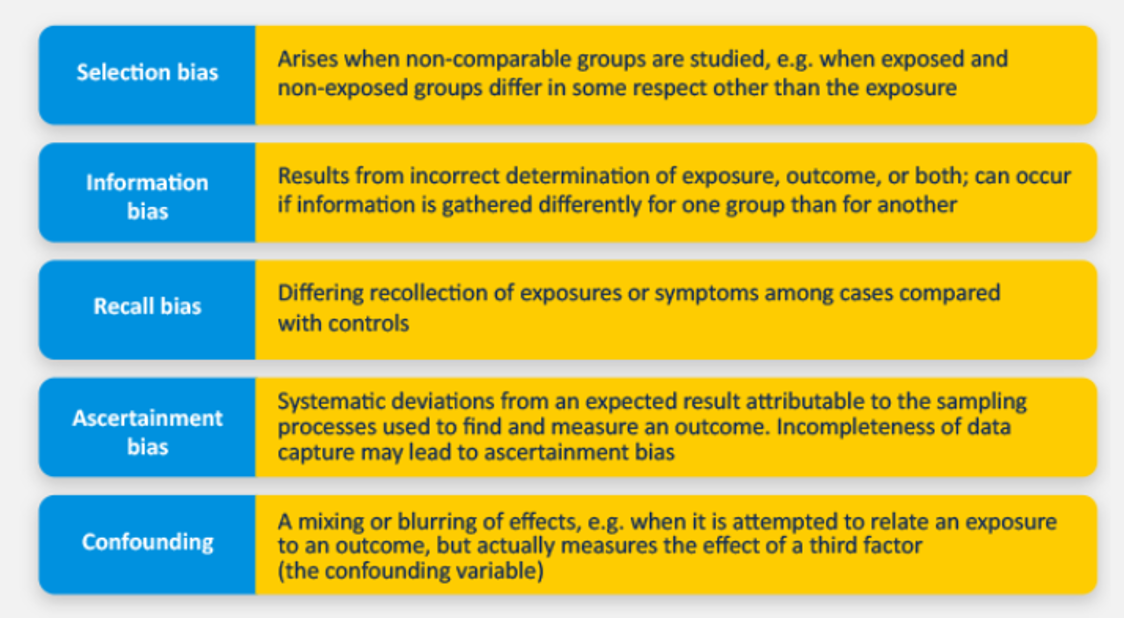
Sources of bias in RWE
Specific biases that can influence RWE quality reflect the generation of data from patients outside the stringently controlled environment of an RCT and are summarised in Figure 1. Appropriate statistical analyses are necessary to control for the presence of biases and confounding factors, to allow robust, clinically relevant conclusions to be made.
Figure 1. Types of bias that can impact the quality of RWD
Strengths and weaknesses of sources of RWD in retinal disease
- RWD can be collected prospectively, to answer a specific research question (known as primary RWD), or retrospectively (known as secondary RWD), and can include collection from multiple sources. In a prospective study, participants are enrolled and followed in time to observe outcomes; in a retrospective study, investigators use pre-existing data to identify participants in the past and follow them forward to determine outcomes. Although potentially restricted by incomplete historical data records, retrospective studies may be quicker and more cost-effective to set up due to use of previously existing data. The strengths and weaknesses of the main sources of RWD in retinal disease are discussed below.
Non-interventional studies
A non-interventional study is one in which the treatment is prescribed in the usual manner, according to usual day-to-day clinical practice patterns, rather than the assignment of a patient to a treatment being decided in advance by a trial protocol. The prescription of a treatment is therefore clearly separated from the decision to include the patient in the study. These studies can be prospective or retrospective and can follow a range of different designs. Some of the most commonly used non-interventional study designs are described below.
- Cohort studies are the most widely used and well-known study designs used in ophthalmology. These studies identify a group of people and follow them over a period of time to see how their exposures affect their outcomes. Prospective designs allow for standardised patient inclusion criteria and calculation of incidence rates, relative risks and attributable risks within a set time period. PERSEUS10 and RAINBOW11 are examples of prospective cohort studies in patients with nAMD while LUMINOUS12 is an example of a combined prospective and retrospective study design.
- Case-control studies are characterised by the identification of patients with the condition of interest and comparison with matched controls. They can be used to investigate any treatment-associated adverse events and assess rare conditions or outcomes, such as post-surgical endophthalmitis.13 These studies are usually retrospective, which typically makes them cost-effective and quick to establish, but they are susceptible to recall bias and confounding factors associated with missing values attributable to poor record-keeping.5,14
Case studies/series typically report on one or a series of patients with the condition of interest;5 for example, case series from Japan have provided data on the effectiveness of intravitreal aflibercept monotherapy in polypoidal choroidal vasculopathy, a subtype of nAMD.3 They can focus on interesting or key elements of disease history and treatment, such as adverse events, or assess treatments and practices not yet studied in RCTs. However, since patient numbers are often low, there is a risk of selection bias that can lead to overestimation or misinterpretation of outcomes.5
Patient registries
Data from patient registries are typically prospectively collected to evaluate specified outcomes for a predefined population. Patients are included in registries via an exposure (drug/medical device/environmental exposure) or via having a certain pre-specified disease. These registries serve predetermined scientific, clinical or policy purposes and can be used to collect post-marketing safety data, understand the natural history of a condition, or assess various qualities of care experienced by patients.7 The Fight Retinal Blindness! (FRB!) project is a registry that tracks RWD on nAMD, choroidal neovascularisation, diabetic macular oedema and retinal vein occlusion from public and private health settings in Australia, New Zealand, Singapore and European countries, including Switzerland, the Netherlands, the UK, Spain, France and Austria. The database is unique in holding 10 years of international data on treatment outcomes for nAMD.5,15,16
Electronic health records
Electronic health records can provide a comprehensive record of an individual’s health and clinical history, including demographic data, medical history, diagnostic and laboratory test results, treatments and procedures. Medisoft Ophthalmology and mediSIGHT are UK electronic health record systems17 that hold information on clinical visits, assessments, ophthalmic procedures and clinical outcomes, and aim to make electronic health record data available for quality control/research purposes. Electronic health records can be used relatively simply to retrospectively compare outcomes between patients treated using different approaches (e.g. different anti-VEGF agents or dosing regimens), but are dependent on the completeness of record-keeping to provide complete datasets.5
Reimbursement claims databases
Reimbursement claims databases provide data on the types and frequency of diagnostic procedures and medications routinely used in clinical practice. Databases comprising data from both public and private systems exist worldwide, such as the US Medicare database18 and the UK Clinical Practice Research Datalink.19 Claims data are a valuable source of large, diverse patient populations that lack selection bias, and longitudinal follow-up data are often available – because of their large size, insights into rare events can be gained from these databases.3 However, there are inherent limitations of claims data, including incomplete, inaccurate, or missing data, the inability to evaluate the appropriateness of care,20 and their primary purpose not being to collect safety and/or effectiveness data.
Patient surveys and questionnaires
Patient surveys can be conducted in person or remotely (electronically or by phone) and can be used to collect patient-relevant data on aspects such as adherence, preferences, functional status and quality of care. For example, the VISION 2020 UK Eye Survey aims to find out about the eye health of 250,000 people living in the UK.21 While patient surveys and questionnaires are able to collect information on outcomes rarely reported in other studies, limitations include introduction of subjectivity on outcome reporting, the potential for survey wording to influence answers, and recall bias.5
Evaluating sources of RWD in retinal disease
The increasing importance of RWE in clinical decision-making means that it is important for practising ophthalmologists to be able to easily evaluate the quality of published RWE and the applicability of findings to clinical practice. In order to do this, simple tools are required to facilitate critical evaluation of published RWE, considering important factors including the data source, study design and analyses in relation to the research question.5
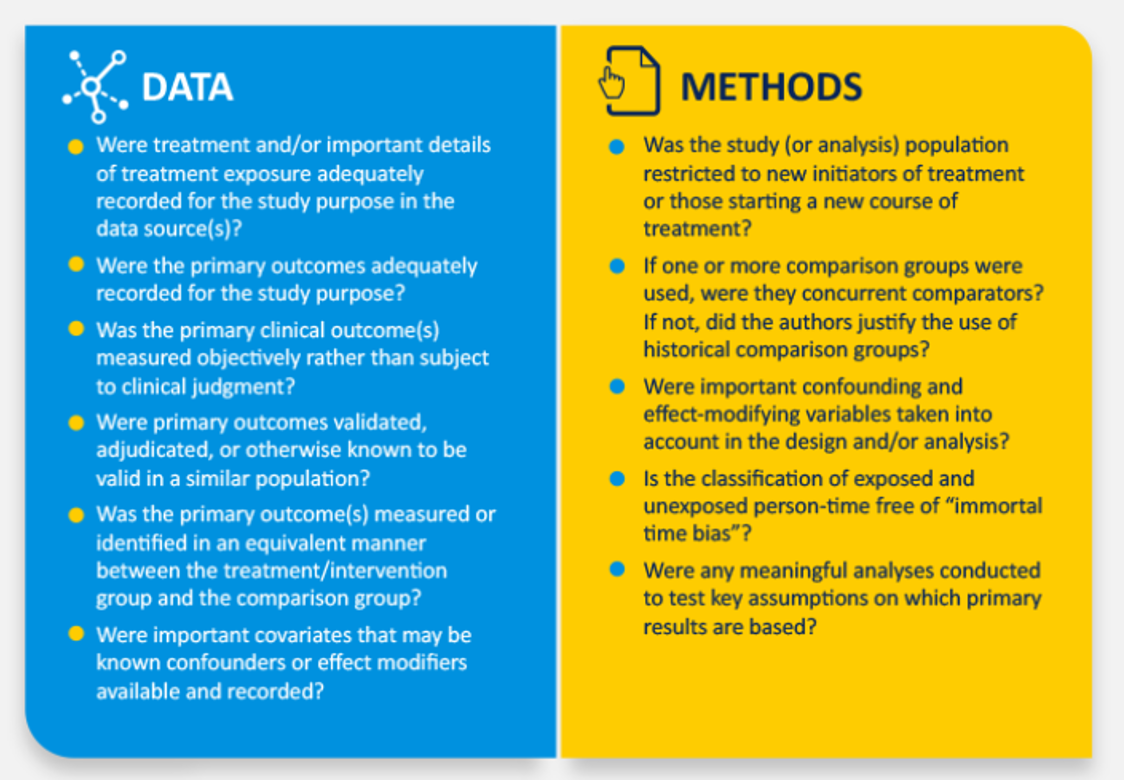
Some resources are available to aid practising ophthalmologists in their evaluation of the quality of RWE. For example, the International Consortium for Health Outcomes Measurement (ICHOM) has defined a minimum set of standardised and patient-oriented outcome measures that should be collected and reported as RWD on macular degeneration. These include patient baseline status, clinical outcomes, patient treatment and management, patient safety, quality of life, and healthcare economics.22 The Good Research for Comparative Effectiveness (GRACE) principles can also be used to support clinicians, researchers, and decision-makers in evaluating the quality of observational comparative effectiveness studies (Figure 2).23 However, availability of a framework to facilitate the systematic assessment of quality and relevance of RWE concerning intravitreal anti-VEGF therapy, specifically, would be valuable. Inclusion of retinal disease-specific considerations, such as method of administration and injection clinic set-up, would help ophthalmologists to more easily and accurately assess the quality of the RWE relating to the use of anti-VEGFs.
Figure 2: GRACE checklist to support ophthalmologists in the evaluation of RWE
Summary
RWE can provide insights into key outcomes in retinal disease as experienced in every-day practice, including long- and short-term effects on vision, as well as patient-reported outcomes. In this way, findings from RWE can positively influence the treatment of retinal disease in clinical practice, for example by providing insights into optimising treatment adherence and injection frequency, to improve and preserve visual acuity.5 Critical evaluation of the method of RWD collection, the subsequent analysis and reporting, and the conclusions drawn are important to permit effective assessment of the quality of published RWE. This enables judgement of the relevance and applicability of RWE to clinical practice and supports confidence in translation of the findings from RWE into clinical practice, to optimise care for patients with nAMD.
References
- Garrison LP, Jr., Neumann PJ, Erickson P, Marshall D, Mullins CD. Using real-world data for coverage and payment decisions: the ISPOR Real-World Data Task Force report. Value in Health: the journal of the International Society for Pharmacoeconomics and Outcomes Research. 2007;10(5):326-335.
- Mehta H, Tufail A, Daien V, et al. Real-world outcomes in patients with neovascular age-related macular degeneration treated with intravitreal vascular endothelial growth factor inhibitors. Progress in retinal and eye research. 2018;65:127-146.
- Talks J, Daien V, Finger RP, et al. The use of real-world evidence for evaluating anti-vascular endothelial growth factor treatment of neovascular age-related macular degeneration. Surv Ophthalmol. 2019:doi: 10.1016/j.survophthal.2019.1002.1008. [Epub ahead of print].
- Berger M, Daniel G, Frank K, et al. White paper: A framework for regulatory use of real-world evidence. 2017.
- Talks J. Utility of real-world evidence for evaluating anti–vascular endothelial growth factor treatment of neovascular age-related macular degeneration. Survey of Ophthalmology. 2018;In press.
- Parke Ii DW, Lum F, Rich WL. The IRIS(R) Registry : Purpose and perspectives. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2017;114(Suppl 1):1-6.
- RWE Navigator. Putting real-world healthcare data to work. Available at: https://rwe-navigator.eu/use-real-world-evidence/sources-of-real-world-data/healthcare-databases-with-a-focus-on-electronic-health-records/.
- Grimes DA, Schulz KF. Bias and causal associations in observational research. Lancet (London, England). 2002;359(9302):248-252.
- Bethesda (MD): National Center for Biotechnology Information (US); 2005. Ascertainment Bias. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9792/.
- Framme C, Eter N, Hamacher T, et al. Aflibercept for patients with neovascular age-related macular degeneration in routine clinical practice in Germany: Twelve month outcomes of PERSEUS. Ophthalmology Retina. 2018;2(6):539-549.
- Weber M, Velasque L, Coscas F, Faure C, Aubry I, Cohen ANobotRsi. Effectiveness and safety of intravitreal aflibercept in patients with wet age-related macular degeneration treated in routine clinical practices across France: 12-month outcomes of the RAINBOW study. BMJ Open Ophthalmology. 2019;Accepted.
- Semoun O, Cohen SY, Srour M, et al. [Individualized management of patients with exudative AMD, IOI protocol: Injection-observational-individualization]. J Fr Ophtalmol. 2017;40(3):169-176.
- S L, P C. Epidemiology in Practice: Case-control studies. Community Eye Health. 1998;11(28):57-58.
- Lewallen S, Courtright P. Epidemiology in practice: case-control studies. Community Eye Health. 1998;11(28):57-58.
- Save Sight Registries. Available at: http://savesightregistries.org/about-us/.
- Save Sight Institute website. Available from: http://www.savesightinstitute.org.au/.
- Medisoft Ophthalmology. Available from: http://www.medisoft.co.uk/medisoft-ophthalmology.
- Centers for Medicare and Medicaid Services. CMS Program Statistics. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/index.html.
- Clinical Practice Research Datalink. Available from: https://www.cprd.com/home/.
- Stein JD, Lum F, Lee PP, Rich WL, 3rd, Coleman AL. Use of health care claims data to study patients with ophthalmologic conditions. Ophthalmology. 2014;121(5):1134-1141.
- VISION 2020 UK. Available from: https://www.opticianonline.net/news/vision-2020-uk-plans-eye-health-survey-1.
- Rodrigues IA, Sprinkhuizen SM, Barthelmes D, et al. Defining a Minimum Set of Standardized Patient-centered Outcome Measures for Macular Degeneration. Am J Ophthalmol. 2016;168:1-12.
- Dreyer NA, Bryant A, Velentgas P. The GRACE Checklist: A Validated Assessment Tool for High Quality Observational Studies of Comparative Effectiveness. Journal of managed care & specialty pharmacy. 2016;22(10):1107-1113.
Eylea Prescribing information
Name of the medicinal product: Eylea 40 mg/ml solution for injection. (Refer to full SmPC before prescribing.) Composition Each vial contains 100 µl, equivalent to 4 mg aflibercept. Excipients: Polysorbate 20, Sodium dihydrogen phosphate, monohydrate, Disodium hydrogen phosphate, heptahydrate, Sodium chloride, Sucrose, Water for injection.
Indication: Eylea is indicated for adults for treatment of neovascular (wet) age-related macular degeneration (AMD), visual impairment due to macular oedema secondary to retinal vein occlusion (branch RVO or central RVO), visual impairment due to diabetic macular oedema (DME) and visual impairment due to myopic choroidal neovascularisation (myopic CNV).
Administration and Dosage: For intravitreal injection only. Each vial should only be used for the treatment of a single eye. Extraction of multiple doses from a single vial may increase the risk of contamination and subsequent infection. Administration only by qualified physician experienced in administering intravitreal injections. Recommended dose: 2 mg aflibercept (0.05 ml) equivalent to 50 microlitres. For wet AMD, treatment is initiated with 1 injection per month for 3 consecutive doses. The treatment interval is then extended to 2 months. Based on the physician’s judgement of visual and/or anatomic outcomes, the treatment interval may be maintained at 2 months or further extended using a treat-and-extend dosing regimen, where injection intervals are increased in 2- or 4-weekly increments to maintain stable visual and/or anatomic outcomes. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly to a minimum of 2 months during the first 12 months of treatment. There is no requirement for monitoring between injections. Based on the physician’s judgement the schedule of monitoring visits may be more frequent than the injection visits. Treatment intervals greater than 4 months between injections have not been studied. For RVO (branch RVO or central RVO), after initial injection, treatment is given monthly. The interval between the 2 doses should not be shorter than 1 month. If visual and anatomic outcomes indicate that the patient is not benefiting from continued treatment, Eylea should be discontinued. Monthly treatment continues until maximum visual acuity is achieved and/or there are no signs of disease activity. Three or more consecutive, monthly injections may be needed. Treatment may then be continued with a treat-and-extend regimen with gradually increased treatment intervals to maintain stable visual and/or anatomic outcomes; however, there are insufficient data to conclude on the length of these intervals. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly. The monitoring and treatment schedule should be determined by the treating physician based on the individual patient’s response. Monitoring for disease activity may include clinical examination, functional testing or imaging techniques (e.g. optical coherence tomography or fluorescein angiography). For DME, initiate treatment with 1 injection/month for 5 consecutive doses, followed by 1 injection every 2 months. No requirement for monitoring between injections. After the first 12 months of treatment, and based on visual and/or anatomic outcomes, the treatment interval may be extended such as with a treat-and-extend dosing regimen, where the treatment intervals are gradually increased to maintain stable visual and/or anatomic outcomes; however, there are insufficient data to conclude on the length of these intervals. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly. The schedule for monitoring should therefore be determined by the treating physician and may be more frequent than the schedule of injections. If visual and anatomic outcomes indicate that the patient is not benefiting from continued treatment, treatment should be discontinued. For myopic CNV, a single injection is to be administered. Additional doses may be administered if visual and/or anatomic outcomes indicate that the disease persists. Recurrences should be treated as a new manifestation of the disease. The schedule for monitoring should be determined by the treating physician. The interval between 2 doses should not be shorter than 1 month.
Contraindications:
Hypersensitivity to aflibercept or to any of the excipients. Active or suspected ocular or periocular infection. Active severe intraocular inflammation.
Warnings and Precautions:
Intravitreal injections have been associated with endophthalmitis, intraocular inflammation, rhegmatogenous retinal detachment, retinal tear and iatrogenic traumatic cataract. Aseptic injection technique is essential. Additionally, patients should be monitored during the week following the injection to permit early treatment if an infection occurs. Patients must report any symptoms of endophthalmitis or any of the above-mentioned events without delay. Increases in intraocular pressure (IOP) were seen within 60 min. of intravitreal injection. Special precaution is needed in poorly controlled glaucoma (no injection while IOP is ≥ 30 mmHg). In all cases, IOP and perfusion of optic nerve head must be monitored and managed appropriately. Potential for immunogenicity. Instruct patients to report any signs or symptoms of intraocular inflammation, e.g. pain, photophobia, or redness, which may be a clinical sign attributable to hypersensitivity. Systemic adverse events including non-ocular haemorrhages and arterial thromboembolic events have been reported following intravitreal injection of VEGF inhibitors. Safety and efficacy of concurrent use in both eyes have not been systematically studied. No data are available on the concomitant use of Eylea with other anti-VEGF medicinal products (systemic or ocular). Risk factors associated with development of retinal pigment epithelial tear after anti-VEGF therapy for wet AMD, include large and/or high pigment epithelial retinal detachment. When initiating therapy, use caution in patients with these risk factors for retinal pigment epithelial tears. Withhold treatment in patients with rhegmatogenous retinal detachment or stage 3 or 4 macular holes. Withhold dose and treatment should not be resumed in event of a retinal break until break is adequately repaired. Withhold dose and do not resume treatment earlier than next scheduled treatment in event of: decrease in best-corrected visual acuity of ≥ 30 letters compared with last assessment; subretinal haemorrhage involving centre of fovea, or, if size of haemorrhage is ≥50%, of total lesion area. Withhold dose within previous or next 28 days in event of performed or planned intraocular surgery. Eylea should not be used in pregnancy unless the potential benefit outweighs the potential risk to the foetus. Women of childbearing potential have to use effective contraception during treatment and for at least 3 months after the last intravitreal injection of aflibercept. Populations with limited data: There is limited experience with treatment of patients with ischaemic CRVO and BRVO. In patients presenting with clinical signs of irreversible ischaemic visual function loss, the treatment is not recommended. There is limited experience in DME due to type I diabetes or in diabetic patients with an HbA1c over 12% or with proliferative diabetic retinopathy. Eylea has not been studied in patients with active systemic infections, concurrent eye conditions such as retinal detachment or macular hole, or in diabetic patients with uncontrolled hypertension. This lack of information should be considered when treating such patients. In myopic CNV there is no experience with Eylea in the treatment of non-Asian patients, patients who have previously undergone treatment for myopic CNV, and patients with extrafoveal lesions.
Undesirable effects:
Very common: Visual acuity reduced, conjunctival haemorrhage, eye pain. Common: Retinal pigment epithelial tear (known to be associated with wet AMD; observed in wet AMD studies only), detachment of the retinal pigment epithelium, retinal degeneration, vitreous haemorrhage, cataract, cataract cortical, cataract nuclear, cataract subcapsular, corneal erosion, corneal abrasion, intraocular pressure increased, vision blurred, vitreous floaters, vitreous detachment, injection-site pain, foreign body sensation in eyes, lacrimation increased, eyelid oedema, injection-site haemorrhage, punctate keratitis, conjunctival hyperaemia, ocular hyperaemia. Uncommon: Hypersensitivity (during the post-marketing period, reports of hypersensitivity included rash, pruritus, urticaria, and isolated cases of severe anaphylactic/anaphylactoid reactions), culture positive and culture negative endophthalmitis, retinal detachment, retinal tear, iritis, uveitis, iridocyclitis, lenticular opacities, corneal epithelium defect, injection-site irritation, abnormal sensation in eye, eyelid irritation, anterior chamber flare, corneal oedema. Rare: Blindness, cataract traumatic, vitritis, hypopyon. Description of selected adverse reactions: In the wet AMD phase III studies, there was an increased incidence of conjunctival haemorrhage in patients receiving anti-thrombotic agents. Arterial thromboembolic events are adverse events potentially related to systemic VEGF inhibition. There is a theoretical risk of arterial thromboembolic events, including stroke and myocardial infarction, following intravitreal use of VEGF inhibitors. As with all therapeutic proteins, there is a potential for immunogenicity.
On prescription only. Marketing Authorisation Holder: Bayer AG, 51368 Leverkusen, Germany.
Date of revision of the underlying Prescribing Information: July 2018.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.