NICE recommends dexamethasone adalimumab for uveitis
The UK’s National Institute for Health and Care Excellence (NICE) has given preliminary approval to dexamethasone 0.7 mg intravitreal implant (Ozurdex, Allergan) and adalimumab (Humira, AbbVie) for sight-threatening non-infectious posterior uveitis.
By Laird Harrison
The UK’s National Institute for Health and Care Excellence (NICE) has given preliminary approval to dexamethasone 0.7 mg intravitreal implant (Ozurdex, Allergan) and adalimumab (Humira, AbbVie) for sight-threatening non-infectious posterior uveitis.
If the cost regulator’s final appraisal determination (FAD) is confirmed as final guidance, the UK’s NHS will be required to offer both treatments as fully funded options for patients where the disease is active and there is worsening vision with risk of blindness.
The treatments would broaden the options for clinicians trying to help patients with a complicated condition. Currently, corticosteroids are the mainstay of treatment for uveitis after underlying conditions, such as infection, are ruled out.
However, systemic corticosteroids can cause severe side effects when used long term. When administered as drops, steroids cannot penetrate the blood-retinal barrier, but intravitreal injections must often be repeated and can also cause side effects, including cataracts and glaucoma.
A surgically placed nonbioerodible implant that releases fluocinolone into the vitreous has proved effective for up to 3 years, but may also lead to cataracts and glaucoma.
Biologic hope
Developed for the treatment of retinal disease, the biodegradable intravitreal implant releases dexamethasone over an extended period.
Adalimumab is not a steroid, but rather a biologic treatment that suppresses tumour necrosis factor alpha, a specific source of inflammation that can have a role in uveitis.
Dexamethasone implants are currently funded for posterior segment uveitis in some parts of the UK but not in others, meaning that access to the treatment can be dependent on where the patient lives rather than clinical needs.
The FAD represents the considered view of NICE’s expert committee as to the cost and clinical effectiveness of these products.
The FAD is subject to appeal, but if there is no appeal, or no appeal is upheld, then it will be published as NICE’s final guidance. This is expected to occur in July. Following publication of the guidance, the NHS must ensure that, within no more than 3 months, it will provide funding for the two treatments in line with the terms of the recommendation.
NICE guidance usually applies only to England and Wales. However, since this guidance is the result of a multiple technology appraisal (where more than one technology is considered in the same review for the same condition), Health Improvement Scotland will also consider whether it should apply to Scotland.
“As final guidance, it would mean improved access to treatments, including [dexamethasone 0.7 mg intravitreal implant] and their availability in places where this was impossible before,” said Jessica Hall, advocacy policy project officer from the Royal National Institute of Blind People, in an Allergan press release.
“Given that the vision loss associated with uveitis is potentially avoidable, it is right that the NHS pays for treatments that NICE has shown are cost and clinically effective in this area,” Hall added.
Preventable
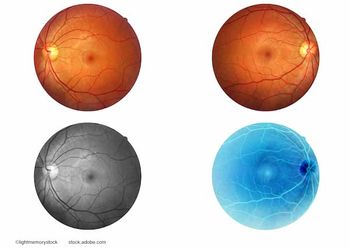
The term uveitis covers a wide range of conditions that can lead to intraocular inflammation and cause about 10% of severe visual impairment. This makes uveitis one of the leading causes of severe preventable visual loss in developed countries.
Non-infectious uveitis is inflammation in the back of the eye that can lead to the appearance of floaters, blurring and decreased vision.
Dexamethasone implants are already approved by NICE for the treatment of adult patients with visual impairment due to diabetic macular oedema (DMO) who are pseudophakic or who are considered insufficiently responsive to, or unsuitable for, non-corticosteroid therapy.
They are also approved for macular oedema following either branch retinal vein occlusion or central retinal vein occlusion.
Adalimumab is approved for use in moderate-to-severe active rheumatoid arthritis; severe active ankylosing spondylitis (AS); severe axial spondyloarthritis without radiographic evidence of AS; moderate to severe chronic plaque psoriasis; active and progressive psoriatic arthritis; moderately to severely active Crohn's disease; moderately to severely active ulcerative colitis; and active moderate to severe hidradenitis suppurativa.
The safety and efficacy of dexamethasone implants in the management of patients with non-infectious uveitis was assessed in a phase III trial known as HURON. The implants provided long-lasting efficacy from a single intravitreal injection, rapid and sustained improvements in vitreous haze and vision, and rapid reductions in macular oedema (ME). They also delivered a manageable safety profile.
Phase II studies, VISUAL-I and VISUAL-II, demonstrated that patients with active and controlled non-infectious intermediate, posterior and panuveitis treated with adalimumab had a significantly lower risk for uveitic flare or decrease in visual acuity, compared with placebo.
No significant differences in adverse events were observed between adalimumab and the
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.














































