Novel factors predict ocriplasmin efficacy in symptomatic vitreomacular traction
Logan Vander Woude, DO, MPH, examines research on improved resolution of symptomatic vitreomacular traction as an attempt to further refine the potential factors predictive of better outcomes.

Reviewed by Logan Vander Woude, DO, MPH, and Gibran S. Khurshid, MD
Improved resolution of symptomatic vitreomacular traction (VMT) has been reported since the introduction of Ocriplasmin (Jetrea, ThromboGenics), with recognition of some factors that predicted better results, including patient age under 65 years, phakic eyes, adhesion diameter smaller than 1,500 microns, and no epiretinal membrane (ERM).1,2
Logan Vander Woude, DO, MPH, and Gibran S. Khurshid, MD, investigators at the Department of Ophthalmology, University of Florida, Gainesville, took a deeper dive into this area of research in an attempt to further refine the potential factors predictive of better outcomes.
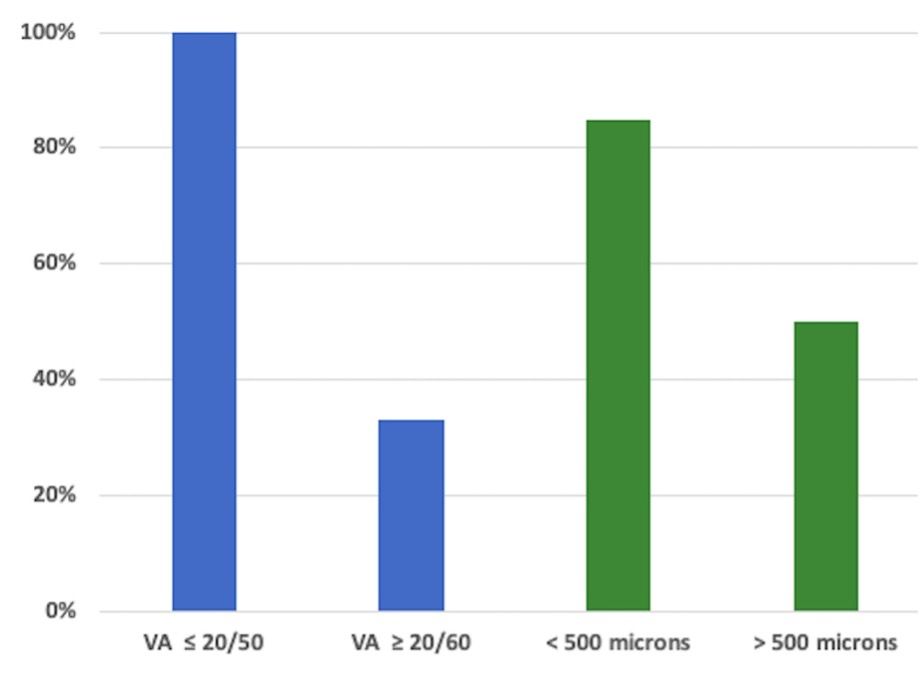
Percent of patients with resolved VMT
They undertook a retrospective analysis of cases of patients with symptomatic VMT at the University of Florida from 2015 to 2020, regardless of lens status, the presence of an ERM, age, and initial visual acuity (VA).
Patients did not undergo Ocriplasmin treatment if they were aphakic, had myopia exceeding 8 D or an axial length exceeding 28 mm, a posterior pole obscured by vitreous opacity, diffuse VMT over 1500 μ, stage 2 or greater macular hole, or other retinal diseases.
The primary outcome measure was the resolution of VMT as seen on optical coherence tomography (OCT) images.
Eleven patients were included in the study. Vander Woude and Khurshid reported that the VMT resolved in 63.6% of cases.
A subgroup analysis showed that the VMT resolved in patients with an initial VA of 20/50 or better.
“These patients did significantly better than those with an initial VA of 20/60 or lower among all patients (p = 0.011) and when controlling for an ERM (p = 0.037).”
A subgroup analysis of micro VMT, defined as less than 500 microns compared with focal VMT, defined as 500 μ to 1500 μ, the former tended to have greater resolution, i.e., 85.7% compared with 50% associated with focal VMT (p = 0.142).
A patient that was considered ideal to undergo Ocriplasmin was a 69-year-old phakic woman who presented with metamorphopsia. The VA was 20/50.
The VMT measured 44 microns and no ERM was present. Two months after treatment, the VMT resolved and the VA improved to 20/25.
“Continued refinement of positive predictor factors is paramount for improving the efficacy of Ocriplasmin and its cost-effectiveness,” the investigators concluded. “While the greater resolution rate in micro VMT was not significant in this small case series, further investigation is warranted. Ocriplasmin may have greater efficacy in patients with symptomatic VMT with VA of 20/50 or better, which may impact useful clinical practice with earlier treatments.”
--
Logan Vander Woude, DO, MPH
E: loganwoude@ufl.edu
This article is adapted from Vander Woude’s presentation at the Association for Research in Vision and Ophthalmology 2021 virtual annual meeting. The authors have no financial interest in this subject matter.
--
References
1. Khan MA, Haller JA. Ocriplasmin for treatment of vitreomacular traction: an update. Ophthalmol Ther. 2016;5:147-59.
2. Haller JA, Stalmans P, Benz MS, et al. Efficacy of intravitreal ocriplasmin for treatment of vitreomacular adhesion: subgroup analyses from two randomized trials. Ophthalmology. 2015;122:117–22.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.