Peripheral retinal drusen more common in Alzheimer’s
People with Alzheimer’s disease are more likely to have drusen in their peripheral retinas, as well as unusual vascular characteristics, researchers believe.
The finding could help prognose the disease and identify people at risk for it, potentially creating a new role for optometrists and ophthalmologists
“We have opened a window to identify high-risk groups who may benefit from specific prevention advice,” said Prof. Craig Ritchie, professor of psychiatry of ageing at the University of Edinburgh, UK, in a university press release.
He and his colleagues reported the finding in
Retinal changes
Previous research dating back to 1986 has linked other changes in the retina to Alzheimer’s disease, including deposition of amyloid plaque, thinning of the retinal fibre layer, signs of impaired vision or abnormal papillary reaction, and tortuoisity of blood vessels.
And such changes have shown up not only in Alzheimer’s but also Parkinson’s disease, multiple sclerosis, amyotrophic lateral sclerosis (ALS), Huntington’s disease and frontotemporal dementia.
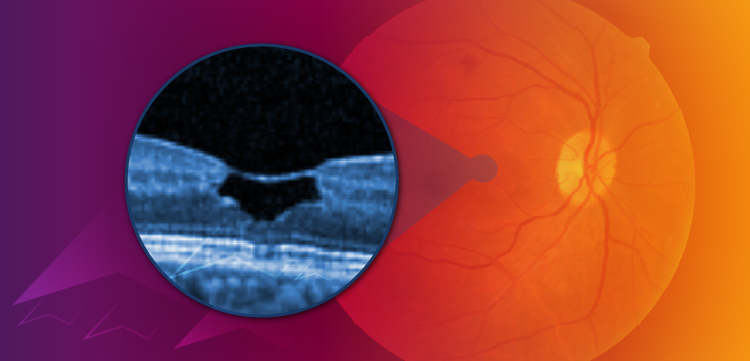
However, exact correlations have remained elusive. One reason may be that researchers focused their attention on the macula, Prof. Ritchie and his colleagues say. Based on laboratory observations, the team hypothesised that changes in the peripheral retina could be more important.
So they used an ultra-wide field scanning laser ophthalmoscope (Optos P200C AF) to study this anatomy. They found a high incidence of drusen in 14 out of 55 people with Alzheimer's, compared to two out of 48 people without Alzheimer’s.
Deposits
Drusen are small deposits of fat, proteins and minerals, including calcium and phosphate deposits that form in a layer underneath the retina. Their incidence increases with age and they are associated with macular degeneration.
They contain amyloid beta, the substance that forms damaging plaques in Alzheimer’s disease, and the process by which drusen and amyloid beta plaques form is similar, according to co-author Dr Imre Lengyel, senior lecturer at the School of Medicine Dentistry and Biomedical Sciences at Queen’s University, Belfast, UK.
The researchers noted potential association between Alzheimer’s disease and age-related macular degeneration in their study, but said their sample size was too small for this to reach statistical significance.
They also noted changes in peripheral retinal blood circulation in the patients with Alzheimer’s. These included wider blood vessels close to the optic nerve that thin faster than in control subjects towards the retinal periphery. Both of these are likely to slow blood flow and impair nutrient and oxygen flow in the peripheral retina, they said.
They speculated that decreased oxygenation could be related to the increased drusen accumulation.
While peripheral retinal imaging is not a diagnostic measure for Alzheimer’s disease, the simple, quick and inexpensive monitoring of changes in the eye could serve as a tool for disease progression in the brain, the researchers said.
“These exciting research results suggests that our original hypothesis was right and wide field eye imaging could indeed help monitoring disease progression in patients with [Alzheimer's],” Dr Lengyel said in the press release. “Eye imaging is quick, simple, well tolerated and costs a fraction to that of brain scans so there are tremendous benefits to both the professional and the patient.”
Planning and monitoring
Catching signs of Alzheimer’s early in the disease will not necessarily confer an advantage in treatment because there are currently no good treatments for the disease, according to researchers. But understanding how rapidly the condition is progressing could help patients and their families plan for future disability.
In addition, it could help researchers monitor the effects of experimental treatments. “Changes in the eye are very easy to measure relative to other measures of brain health,” said Prof. Ritchie.
To extend these observations, the research team plans to follow patients with very early stage Alzheimer’s to see how the disease progression is reflected in their eyes.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.