Research offers insights on clinical course, management of CSCR
By Cheryl Guttman Krader;Reviewed by Francine Behar-Cohen, MD
Acute central serous chorioretinopathy (CSCR) resolves within six months in the majority of patients, but findings from new research suggests ways to identify individuals at risk for longer duration and a new approach to treating patients with severe chronic CSCR with epitheliopathy.

Dr. Behar-Cohen
“Only a subset of patients with CSCR will have a long episode,” said Francine Behar-Cohen, MD, professor of ophthalmology, University of Paris Descartes and Cochin Hospital, both of Paris, France. “These patients are the ones who need to be identified for treatment and when evaluating therapy. In addition, it is important to be able to identify individuals at risk for recurrence because recurrence leads to long-term visual impairment.”
To identify factors predicting a longer episode duration, Dr. Behar-Cohen and colleagues analyzed data from 31 consecutive patients with a first episode of acute CSCR and symptom duration <20 days. The patients had a mean age of 40 years and 84% were male.
Mean time to resolution was 83 days, and CSCR resolved by 6 months in 26 (84%) eyes. By 3 months, however, 52% of the cases had resolved.
Numerous variables analyzed
Results of analyses that considered a number of demographic, clinical, and imaging variables found that age >40 years, subfoveal choroidal thickness ≥500 µm, and retinal pigment epithelium (RPE) elevation ≥50 µm predicted a longer duration of a first CSCR episode.
Data from 46 patients with a mean follow-up of 30 months after an initial episode were analyzed to identify factors associated with CSCR recurrence. Of this cohort, 20 patients (43%) developed a recurrence at a mean of 7 months after resolution of their first episode.
Patients with a shorter interval between resolution of their first episode and their first recurrence had more recurrences, and final visual acuity was worse in patients with more recurrence. Factors associated with recurrence included increased subfoveal choroidal thickness, low fluorescein leakage intensity, meaning low perfusion of the choriocapillaris, and shift work (circadian disruption).
“The factors we identified for longer duration episodes and higher risk of recurrence should be confirmed in larger cohorts and probably also in different ethnic groups,” said Dr. Behar-Cohen.
CSCR management
Dr. Behar-Cohen and colleagues have proposed the use of an oral mineralocorticoid receptor antagonist (MRA, eplerenone or spironolactone) to treat severe chronic CSCR with epitheliopathy along with the addition of a topical corticosteroid in patients who are refractory to the MRA.
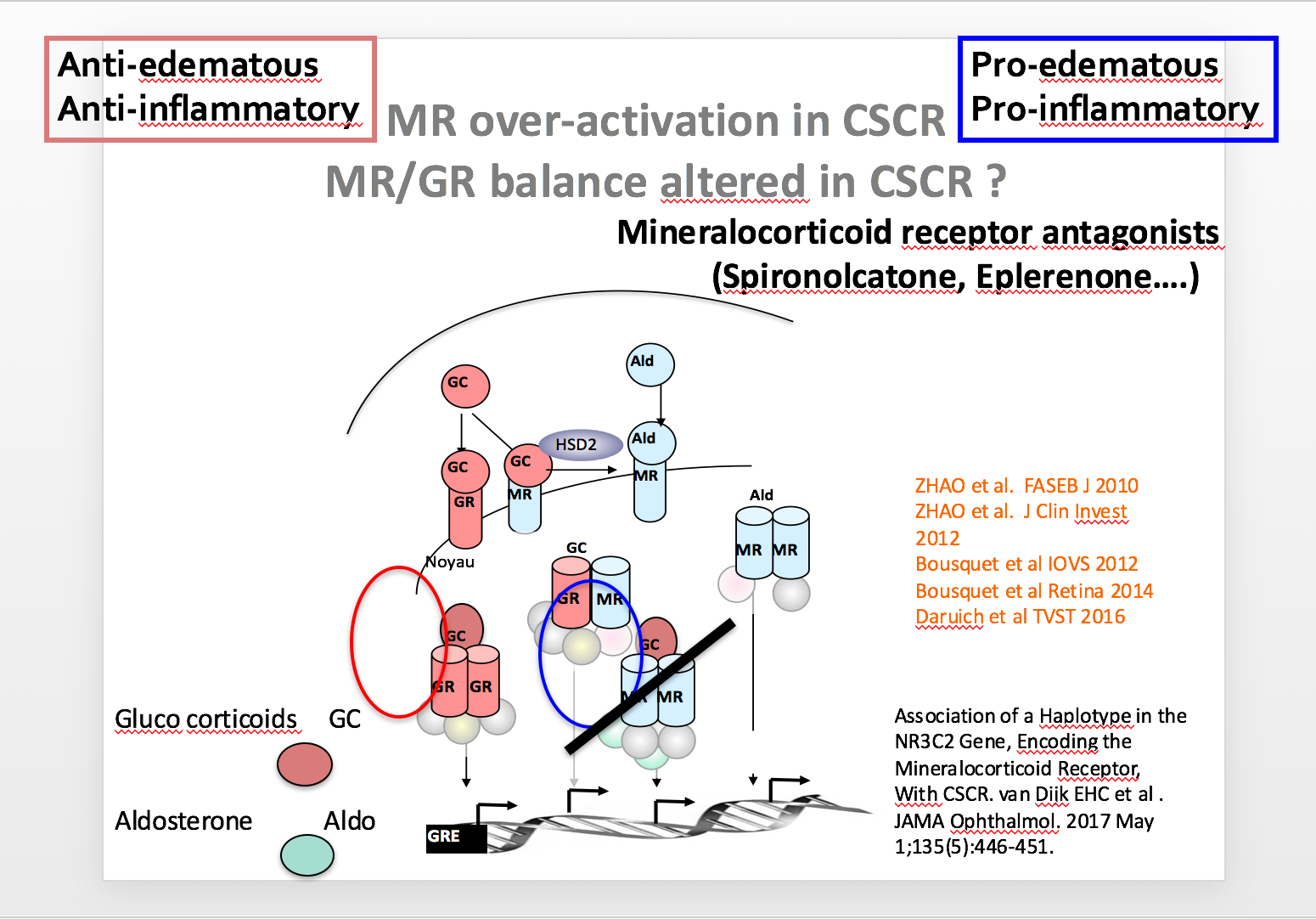
“Although corticosteroids have anti-inflammatory and anti-edematous effects, they have pro-inflammatory and pro-edematous activity when they bind to the mineralocorticoid receptor (MR),” said Dr. Behar-Cohen. “Our proposal for treating CSCR with an MRA is based on the hypothesis that the MR pathway is overactivated in patients with CSCR, and in fact that has been confirmed by genetic studies.”
Treatment with an oral MRA has been successful in some patients with chronic CSCR and diffuse retinal pigment epitheliopathy.
“We found that it may be necessary to use this treatment for a long time, as some patients did not have benefit for more than 6 months,” said Dr. Behar-Cohen.
A potential role for adding topical dexamethasone when patients are refractory to treatment with MRA monotherapy is supported by findings of a single center pilot study. The investigation included 21 patients who had persistent subretinal fluid after treatment with a MRA for >6 months (mean 10.5 months). By 1 month after starting treatment with 3 drops of topical dexamethasone per day, almost all patients benefited with a significant decrease of subretinal fluid and central macular thickness.
“Best corrected visual acuity did not improve significantly in these patients, but most of them were very severe cases,” Dr. Behar-Cohen said. “Further study is needed to confirm the benefit of this regimen.”
Francine Behar-Cohen
This article is based on a presentation given by Dr. Behar-Cohen at the 2017 Retina Subspecialty Day held prior to the 2017 American Academy of Ophthalmology. Dr. Behar-Cohen is the inventor in patents on the use of mineralocorticoid receptor antagonists for retinal diseases. The patent belongs to her employers, Inserm and University of Paris Descartes.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.