Retina risk app tool empowers diabetic patients worldwide
A novel and free app has been developed to help diabetic patients assess their risk for the development of diabetic eye disease and set goals accordingly.
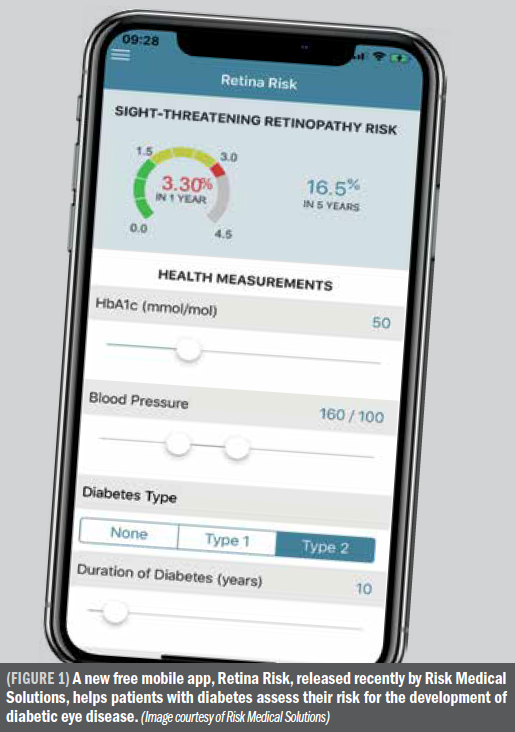
A new tool (Retina Risk App, Risk Medical Solutions [RMS]) helps patients with diabetes assess their risk for the development of diabetic eye disease. What sweetens this news even more is that the app is free and usable with both Android and iOS platforms.
“This mobile app should empower patients to better understand their own risk profiles for eye disease and motivate them to modify their personal risk factors,” said Einar Stefánsson, MD, PhD, professor of ophthalmology and physiology, University of Iceland, National University Hospital, ReykjavÃk, and one of the co-founders of RMS.
The availability and importance of a tool such as this is underscored by how pervasive diabetes has become.
“The global diabetes epidemic has tripled since 2000, to some 430 million persons worldwide, and is expected to exceed 600 million by 2045,” Dr. Stefánsson noted. “Two-thirds of persons with diabetes develop diabetic retinopathy and one-third develop sight-threatening diabetic retinopathy over 20 years. These patients are at high risk of visual impairment or even blindness if not diagnosed and treated in a timely manner.”
The upside to this scenario is that routine eye screening and preventive treatment dramatically reduce blindness that develops as the result of diabetes, which is where the app comes into play.
“The Retina Risk App is a clinically validated risk calculator that allows people with diabetes to assess in real-time their individualized risk for development of sight-threatening diabetic retinopathy, based on their risk profile,” said Arna Gudmundsdottir, MD, diabetologist at Landspitali University Hospital, Department of Endocrinology, the National University Hospital, Reykjavik, Iceland, and also co-founder of RMS.
RELATED: Image-reading accuracy Increases with deep-learning DR algorithms
The app includes detailed guidelines and useful information on diabetes, diabetic retinopathy, and improved self-care, and helps patients to better understand their condition and become active participants in their own wellness journey, they commented.
Key features of the app include individualized and free risk assessment for diabetic retinopathy; customized, easily understandable information with clear guidelines; patient educational material that improves diabetes management and quality of life; ability to track progress; ability to export and share results; and goal setting.
The major characteristic of the app is it empowers patients with diabetes to become more involved in their healthcare decision making. This fits well with the latest American Diabetes Association/European Association for the Study of Diabetes consensus guidelines on management of hyperglycemia that have a special emphasis on patient-centered care and shared decision-making.
The tool supports patient self-management by demonstrating the importance of regular eye examinations and seeking timely medical assistance. The app motivates them to become more responsible and better informed, and its educational tools demonstrate how improvement of modifiable risk factors, e.g., blood glucose, haemoglobin A1c, and blood pressure, can significantly lower the risk of serious diabetic eye disease and expensive interventions, according to Dr. Stefánsson and Dr. Gudmundsdottir.
RELATED: Deep learning predicts OCT measures of diabetic macular thickening
The app algorithm
The proprietary algorithm used in the app was validated clinically in 20,000 persons with diabetes and the results published in several medical journals that are accessible on the app website. The algorithm calculates patients’ annualized risk of developing sight-threatening diabetic retinopathy based upon major, well-established risk factors for the development of sight-threatening diabetic retinopathy.
The algorithm was validated clinically in Northern European diabetes cohorts, which include a variety of races and ethnicities.
Future validation in other populations is planned. The investigators explained that the processes implicated in sight-threatening diabetic retinopathy in all populations depend predominantly on metrics in the algorithm that include blood glucose control and status, blood pressure, disease duration, gender, diabetes subtype, and the presence or absence of non-proliferative retinopathy.
While the algorithm accounts for 80% of established risk in patients with diabetes based upon a preponderance of research data, there are other emerging factors including obstructive sleep apnea, obesity, and a history of other diabetes complications, that probably account for some of the remaining risk and may very well be important for refinement of predictive power.
RELATED: Obesity + diabetic retinopathy: Korean study explores inverse association
More detailed analysis of the fundus image, for example, with artificial intelligence and the addition of oximetry is likely to further increase the power of the personal prediction from the current 80% to well over 90%.
“The personalized report form generated for each patient should allow healthcare providers to communicate the presence of at least some of these emerging risk factors and recommend additional preventative strategies for patients based upon clinical judgment and new research findings,” Dr. Stefánsson said.
The app also answers frequently asked questions that help educate patients about their diabetes and diabetic retinopathy.
“Our vision is to improve diabetes care and transform diabetes education and care by applying technology and epidemiologic data to improve outcomes, focus on patients at the highest risk, and save money,” Dr. Stefánsson concluded. “This is mobile, digital health at the users’ fingertips.”
Information about the Retina Risk App, which currently is available in 23 languages, can be accessed at https://www.retinarisk.com/about/.
RELATED: DNA analysis: Unraveling role of genetics in DR pathogenesis
Disclosures:
Einar Stefansson, MD, PhD
E: einarste@landspitali.is
Dr. Stefánsson is professor of ophthalmology and physiology, University of Iceland, National University Hospital, ReykjavÃk, Iceland.
Arna Gudmundsdottir, MD
E: arnagu@landspitali.is
Dr. Gudmundsdottir is a diabetologist at Landspitali University Hospital, Department of Endocrinology, the National University Hospital, Reykjavik, Iceland.
Dr. Stefánsson and Dr. Gudmundsdottir cofounded RMS in 2009.
References:
Einar Stefansson, MD, PhD
E: einarste@landspitali.is
Dr. Stefánsson is professor of ophthalmology and physiology, University of Iceland, National University Hospital, ReykjavÃk, Iceland.
Arna Gudmundsdottir, MD
E: arnagu@landspitali.is
Dr. Gudmundsdottir is a diabetologist at Landspitali University Hospital, Department of Endocrinology, the National University Hospital, Reykjavik, Iceland.
Dr. Stefánsson and Dr. Gudmundsdottir cofounded RMS in 2009.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.