Rheumatologic–ophthalmologic teams may be needed to improve management of patients with rheumatic diseases
Austrian investigators advise establishing an interdisciplinary setting, ie, rheumatologic–ophthalmologic, to improve management of patients with rheumatic diseases.
Austrian investigators advise establishing an interdisciplinary setting, ie, rheumatologic–ophthalmologic, to improve management of patients with rheumatic diseases.1 The investigators were led by first author Ralf Altenberger, MD, from Clinic II, Department of Internal Medicine, Medical University of Innsbruck, and colleagues from the Department of Ophthalmology and Optometry, Medical University of Innsbruck, Austria.
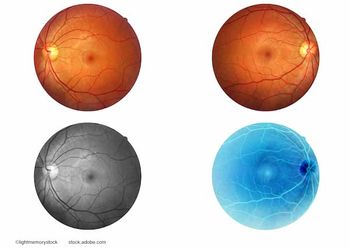
The investigators pointed out that spondyloarthritis (SpA) and Behçet’s disease are typical diseases that require the expertise of rheumatologists and ophthalmologists. Uveitis is a recognized extraskeletal manifestation of both SpA2 and Behcet’s disease.3 However, at least 10 other inflammatory rheumatic diseases are potentially associated with uveitis.4
They commented, “Additionally, there are many more ocular manifestations that possibly present with a rheumatic disease, from keratoconjunctivitis sicca in Sjögren’s syndrome to visual disturbances and even visual loss in giant cell arteritis. Thus, eye involvement in rheumatic diseases may have a dramatic impact on the prognosis and quality of life of patients with rheumatic diseases, whereas other eye diseases may occur independently of rheumatic disease.”
Because there are few data on the prevalence of ocular diseases in patients with rheumatologic diseases, the aims of this study were two-fold: to provide data on the retrospectively assessed prevalence of ophthalmologic diseases in real-world data from a rheumatology outpatient clinic and to consider the role of a multi-disciplinary rheumatology–ophthalmology clinic.
The investigators performed a chart review in this retrospective observational cohort study and reported the following: Of the 1,529 rheumatic outpatients, 26.9% had an ophthalmic diagnosis; whereas from a rheumatologic perspective, inflammatory non-infectious diagnoses dominated at 71.7%. From an ophthalmologic perspective, diagnoses without inflammatory pathophysiologic backgrounds dominated at 54.9%. An inflammatory non-infectious ophthalmologic disease was diagnosed in 24.2% of patients with rheumatoid arthritis and 29.3% of patients with peripheral SpA. Not 1 patient with rheumatoid arthritis was diagnosed with anterior uveitis; however, 16.5% of patients with SpA were diagnosed with anterior uveitis, which was significant (p < 0.001). The prevalence of uveitis was 16.3% in axial and 20.1% in peripheral SpA.
The investigators concluded that an interdisciplinary rheumatologic–ophthalmologic setting appears justified to further improve the management of patients with rheumatic diseases.
References
Altenberger R, Rauchegger T, Haas G, et al. Eye disease in patients with rheumatic diseases: a retrospective observational cohort study. J Clin Med. 2023;12:7510;
https://doi.org/10.3390/jcm12247510 Dougados M, Baeten D. Spondyloarthritis. Lancet 2011:377:2127–2137.
Davatchi F, Chams-Davatchi C, Shams H, et al. Behcet’s disease: epidemiology, clinical manifestations, and diagnosis. Expert Rev. Clin. Immunol. 2017;13:57–65.
Petris CK Almony, A. Ophthalmic manifestations of rheumatologic disease: diagnosis and management. MO Med. 2012;109:53–58.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.














































