The spectrum of central serous retinopathy

Central serous retinopathy (CSR) is a heterogeneous disease with different phenotypes. Multimodal imaging is one way to understand more about the pathogenesis of the disease, and can be used to guide treatment.
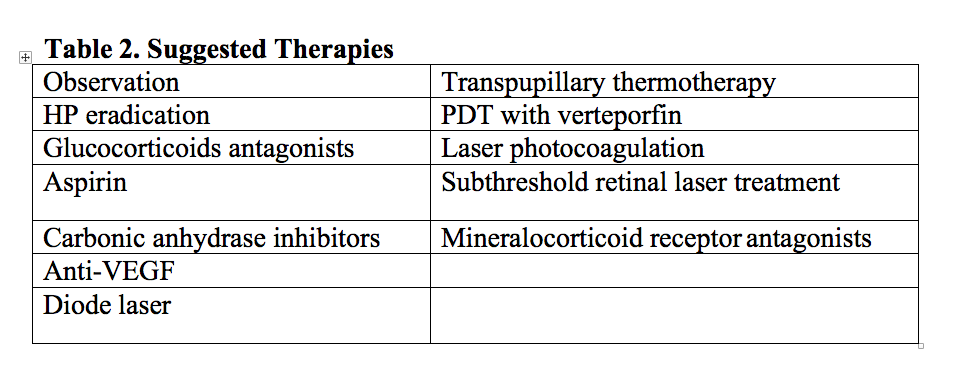
CSR is highly prevalent, especially in Eastern countries. Different treatments have been suggested but none of them have demonstrated universal efficacy for the different phenotypes of the disease.
Giuseppe Querques, MD, presented two cases. The first was a case of an acute form of CSR. The patient was followed for three months with no intervention. There was no spontaneous resolution, so the patient was treated with eplerenone, a mineralocorticoid receptor (MR) antagonist, for three months.
The OCTA showed the appearance of choriocapillaris, and the ICG disclosed the presence of a hotspot that was interpreted as an actively leaking stage of the disease.
Why eplerenone?
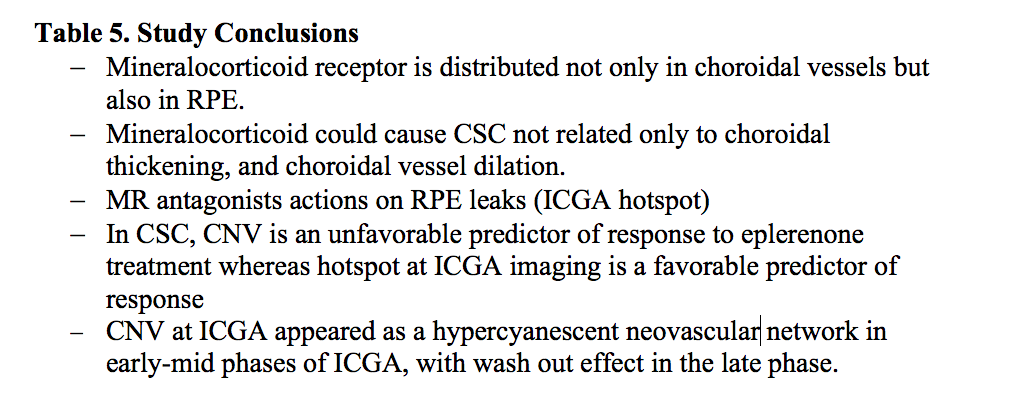
The decision to try eplerenone was based on basic science. The role of a mineralocorticoid on the pathogenesis of a central serous-like pattern has been demonstrated in rats. And treatment with an MR antagonist seems to revert the disease. However, looking at the actual clinical application of MR antagonists, there is a high variability in the response.
To try to further understand this variability, the second case presented was a case of a more chronic form of the disease. Again the patient did not experience spontaneous resolution. The structural OCT showed not only a serous retinal detachment but also a flat irregular RPE elevation. The patient was treated with eplerenone and had no changes in the subretinal fluid, so half fluence PDT was performed, and there was complete resolution of the exudation.
The OCTA showed the irregular elevation of RPE as seen on structural OCT that actually corresponds to choroidal neovascularization. This CNV should be confirmed by ICG. Differently from what is understood about AMD, this type of neovascularization does not show a late plaque on ICG. This was also demonstrated in cases without exudation.
Indocyanine green angiography showed that the network seen on hypofluorescence corresponds to the network visualized on OCT. So for challenging cases, when there is suspicion of CNV, combining these modalities may be helpful.
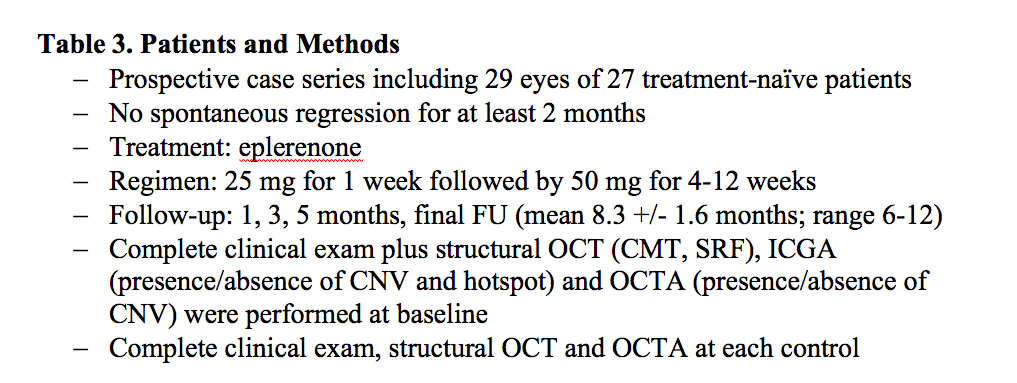
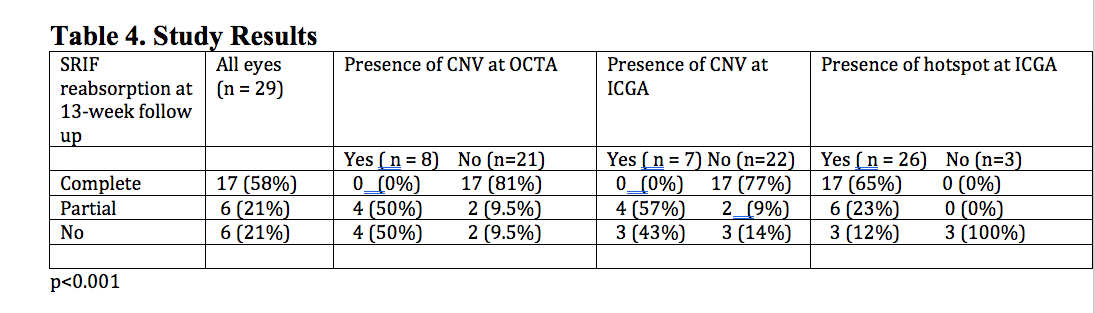
In a series of 29 eyes of 27 treatment-naïve patients by Dr. Querques and colleagues, all cases were treated with eplerenone after at least two months without spontaneous resolution.
Based on the study results, the authors believe the response can be predicted, so that there is now a biomarker that can indicate when treatment with eplerenone will likely be effective.
When CNV is present on OCTA, there appears to be no response to eplerenone, particularly if there is no hotspot on ICG. If there is a hotspot on ICG however, there can be close to complete resolution of subretinal fluid.
Looking at the conclusions of the study, choroidal thickening may not be the only thing responsible for the accumulation of subretinal fluid in the CSR phenotype. RPE that express the receptor for mineralocorticoid may also play an important role in the pathogenesis of the disease, and this may be represented by what is appearing as a hotspot.
Conclusion
The cases and the series presented here show that by using multi-modal imaging, in particular ICG and OCTA, when treating CSR, the response to using eplerenone can be predicted, which can help guide treatment choices.
Disclosures:
Giuseppe Querques, MD, is a consultant to Alimera Sciences, Allergan, Bayer Healthcare Pharmaceuticals, Carl Zeiss Meditec. Heidelberg Engineering, Novartis Pharmaceuticals Corp., and Sandoz.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.