Subretinal gene therapy for neovascular AMD showing efficacy and safety
Novel option demonstrates stable to improved visual acuity and retinal thickness
This article was reviewed by Dante J. Pieramici, MD.
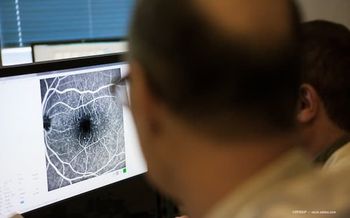
After 1 to 2 years of follow-up in a phase 1/2a dose-escalation study, RGX-314 subretinal gene therapy (ReGenXBio) for neovascular age-related macular degeneration (AMD) continues to be generally well-tolerated and is demonstrating a durable treatment effect with stable to improved visual acuity and retinal thickness as well as meaningful reductions in anti-VEGF injection burden, according to Dante J. Pieramici, MD.
RGX-314 uses a novel adeno-associated viral vector (AAV8) to deliver a gene for an anti-VEGF monoclonal antibody fragment to achieve sustained protein production by retinal cells, said Pieramici, a retina specialist in private practice, California Retina Consultants, Santa Barbara, California.
“A pivotal trial of subretinal RGX-314 gene therapy for neovascular AMD will be starting in 2021,” he said. “A phase 2 clinical trial (AAVIATE) is exploring RGX-314 delivered via a suprachoroidal route as treatment for neovascular AMD. A phase 2 study is investigating suprachoroidal RGX-314 as treatment for diabetic retinopathy without center involved-diabetic macular edema.”
The phase 1/2a trial of subretinal RGX-314 for neovascular AMD enrolled 42 patients across 5 dose cohorts (3 x 109 to 2.5 x 1011 GC/eye). Patients eligible for the study previously were treated with anti-VEGF agents and showed a response and most required very frequent injections to maintain disease control.
After undergoing vitrectomy and subretinal injection of RGX-314, patients were followed every 4 weeks. They were eligible to receive an anti-VEGF injection at the discretion of the investigator if they had increased, new or persistent choroidal neovascularization-related fluid, vision loss greater than or equal to 5 letters associated with fluid, or new ocular hemorrhage.
The baseline characteristics of the patients in the 5 dose cohorts were similar. Mean age was 80 years, mean BCVA was 55.7 ETDRS letters, mean central retinal thickness (CRT) was 399.1 μm, and patients had received an average of approximately 33 previous anti-VEGF injections for an annualized rate of approximately 9.6. Approximately 43% of patients had neutralizing antibodies to AAV8.
Giving an update on the phase 1/2a study results, Pieramici presented data from follow-up to 2 years in the first 3 dose cohorts and from 1 year in the 2 highest dose cohorts. The primary endpoint of the study is focused on safety, and so far, there had been only a single serious adverse event that was considered possibly drug-related. The event occurred in a patient in the highest dose cohort who developed increase of existing retinal pigmentary changes involving the macula and a significant decrease in vision.
Retinal pigmentary changes represented the most common ocular adverse event recorded in the study (76%). Most (70%) were mild and only 1 was severe. Mild postop inflammation developed in approximately one-third of patients and resolved within days to weeks.
Efficacy evidence
Mean BCVA and mean CRT in the first 3 dose cohorts were relatively stable throughout the first year of follow-up. The mean annualized number of injections was unchanged in the first 2 dose cohorts but decreased to just 2.2 in cohort 3. During the second year, BCVA in the 2 lowest dose cohorts remained relatively stable. However, BCVA improved in the third dose cohort (+14 letters from baseline) with receipt of a mean of 2.8 annualized injections.
“The mean annualized injection burden in cohort 3 was reduced by 68% during the first year following RGX-314 administration and by more than 60% during year 2,” Pieramici explained.
In the 2 highest dose cohorts, mean BCVA was relatively stable during the year of available follow-up, and mean CRT showed a modest decrease at 1 month and remained stable thereafter. Mean change from baseline CRT was +61 μm in cohort 4 and -79 μm in cohort 5. BCVA was stable in cohort 4 but improved modestly in cohort 5, which had an 84% reduction in mean annualized anti-VEGF injection burden.
RGX-314 protein levels measured in aqueous samples showed a dose-dependent response across the five dose cohorts (range 2.2 ng/mL to 457.5 ng/mL) and remained relatively stable during 2 years of follow-up in cohort 3 and during the year of follow-up available for cohorts 4 and 5. Baseline serum neutralizing antibodies to AAV8 did not affect RGX-314 protein production, Pieramici concluded.
Dante J. Pieramici, MD
E: dpieramici@yahoo.com
This article is based on Pieramici’s presentation at the 2020 virtual annual meeting of the American Academy of Ophthalmology. Pieramici is a consultant for and receives research funding from ReGenXBio.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.