Topical squalamine offers novel, promising therapy for nAMD
By Cheryl Guttman Krader; Reviewed Jason S. Slakter, MD; Glenn L. Stoller, MD, and David M. Brown, MD
Topical squalamine (Ohr Pharmaceutical), a small molecule being investigated for the treatment of neovascular age-related macular degeneration (nAMD) and other retinal vascular diseases, represents a novel therapy because of its mode of administration and multimodal mechanism of anti-angiogenic activity.
Glenn L. Stoller, MD, chief scientific officer, Ohr Pharmaceutical, New York, outlined the mechanism of action of squalamine. He explained that it is a calmodulin-binding molecule that acts within vascular endothelial cells.
The molecule enters the cells through cell membrane invaginations known as caveolae. Inside the cell, squalamine sequesters calmodulin away from its receptors and causes global suppression of calmodulin-dependent signaling that results in inhibition of VEGF- and basic fibroblast growth factor (bFGF)-mediated cell signaling, as well as decreased expression of cell surface integrins.
Different mode of action
Dr. Stoller differentiated squalamine’s anti-VEGF mode of action from that of existing anti-VEGF therapies.
“The clinically available anti-VEGF agents used to treat retinal diseases are VEGF ligand binding agents that prevent VEGF from binding to its receptor, but they cannot prevent cell signaling induced by VEGF that is able to bind to the VEGF receptor,” Dr. Stoller said. “With its different mechanism of action, squalamine can block all of the downstream effects that occur after VEGF binds to its receptor.”
Blockade of bFGF is also an important component of squalamine’s activity because bFGF is a potent mitogen for vascular endothelial cells and for fibroblasts that mediate the fibrosis that can occur with wet AMD, he added. The significance of decreasing integrin expression is that integrins are overexpressed on endothelial cells during angiogenesis and facilitate the growth and survival of the newly forming vessels.
Dr. Stoller explained that because it is an amphiphilic molecule, topically applied squalamine is able to penetrate to the posterior segment through a transscleral route and reach therapeutic concentrations in the choroid where it has a prolonged intracellular half-life.
“Squalamine happens to be particularly ‘sticky’ to the choroid because of its cationic side chain,” Dr. Stoller said.
Phase III study update
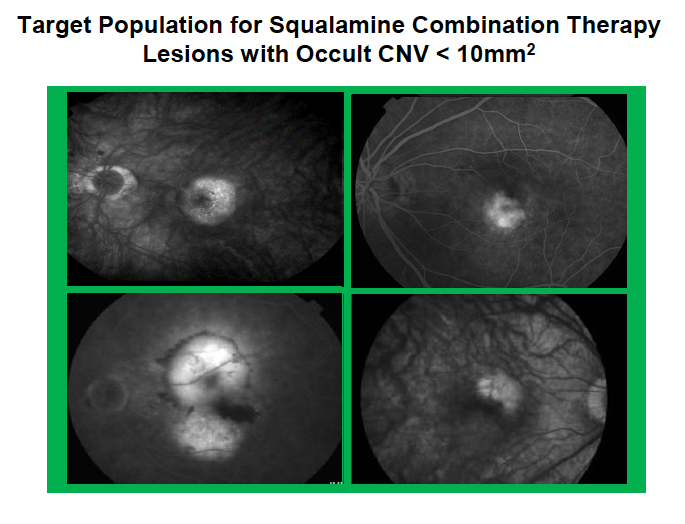
The clinical development program for topical squalamine includes studies for the treatment of nAMD, diabetic macular edema, proliferative diabetic retinopathy, and macular edema related to retinal vein occlusion. MAKO, a randomized, double-masked, placebo-controlled clinical trial investigating squalamine lactate 0.2% ophthalmic solution twice daily with anti-VEGF therapy is underway.
In MAKO, eligible patients were assigned to treatment with intravitreal ranibizumab (Lucentis, Genentech) every 4 weeks plus topical squalamine or placebo ophthalmic solution twice daily for 9 months.
Improvement in ETDRS best-corrected visual acuity (BCVA) from baseline to month 9 is being analyzed as the primary endpoint.
“Newly diagnosed wet AMD is characterized by the presence of very active blood vessels, and that supports our strategy to initiate therapy with a combination, multi-targeted treatment regimen,” said Jason S. Slakter, MD, chief executive officer, Ohr Pharmaceuticals. “We are looking forward to the primary efficacy data readout that we expect will occur in early 2018.
“Additional clinical trials, however, will be designed to include investigating whether squalamine by itself might be used to maintain stability once disease activity is controlled and vision is improved,” he added.
Dr. Slakter pointed out that the company’s future plans also include studying squalamine as a non-invasive standalone treatment to prevent conversion from dry to wet AMD in high-risk eyes.
Clinician's viewpoint
David M. Brown, MD, clinical professor of ophthalmology, Baylor College of Medicine; vice chairman for research at the Blanton Eye Institute, Houston Methodist Hospital; and chairman of the Steering Committee for the squalamine MAKO clinical program, spoke to the medical need for a non-invasive alternative to intravitreal anti-VEGF treatment.
“I treat 30 to 50 people a day with anti-VEGF therapy for AMD and other diseases,” Dr. Brown said. “The need to come for monthly injections is a real burden for patients.”
Dr. Brown said that while the possibility of achieving greater improvement in visual acuity by adding squalamine to anti-VEGF therapy is being looked at as the primary endpoint in MAKO, the exciting aspect of squalamine for patients and clinicians will be if its use enables a decrease in anti-VEGF dosing frequency.
“Therefore, we are particularly looking forward to the results from the extension of the study past the primary endpoint.” He added that so far, topical squalamine has exhibited a favorable safety profile.
“To date, no safety signals have emerged,” Dr. Brown said. “Although I am masked to whether patients in MAKO are receiving squalamine or placebo, we are not seeing problems with ocular stinging or burning that can occur with topical treatments.”
David M. Brown, MD
Jason S. Slakter, MD
e. jslakter@ohrpharmaceutical.com
Glenn L. Stoller, MD
e. gstoller@ohrpharmaceutical.com
Dr. Brown is a consultant for Ohr Pharmaceutical and receives research support for clinical research trials from Ohr Pharmaceutical. Dr. Stoller is the chief scientific officer and a consultant to Ohr Pharmaceutical. Dr. Slakter is an employee and chief executive officer of Ohr Pharmaceutical.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.