Trending Now: Hottest surgery stories of 2014
The hottest stories in surgery this year included news about cataract surgery by a charity-run Indian camp cost at least 24 elderly people their eyesight, how to correct RK, and how to identify and manage dysphotopsia after cataract surgery.
1. Cataract surgery by charity-run camp costs at least 24 elderly people their eyesight
Earlier this month, we reported that a physician who conducted cataract surgeries on 130 poor and elderly people at a health camp in the northern Indian state of Punjab has been arrested. At least 24 people lost their eyesight following free cataract surgery at the health camp, which was organized by a nonprofit. The government has launched an investigation into the matter.
Ophthalmology Times Editorial Advisory Board Member Ashley Behrens, MD, shared her thoughts on this international story.
“This is a very unfortunate event occurring in a setting where additional precautionary measures should have been taken. Although we do not know the facts in detail in this case, postoperative endophthalmitis is a complication that can be effectively prevented using strict, standard protocols," she said. "The rates of endophthalmitis in modern cataract surgery fluctuate between 1 in 500 to 1,000 cases, depending on the series."
"I personally had the chance to participate in several charity campaigns in the past, and our numbers of postoperative endophthalmitis were very close to the published literature," Dr. Behrens continued. "This is a sad case that requires further investigation to determine possible causes and accountability. Underprivileged populations deserve the same high quality of care, even more under these special campaigns."
2. Entering the Lion’s Cage: Correcting RK-A refractive epidemic
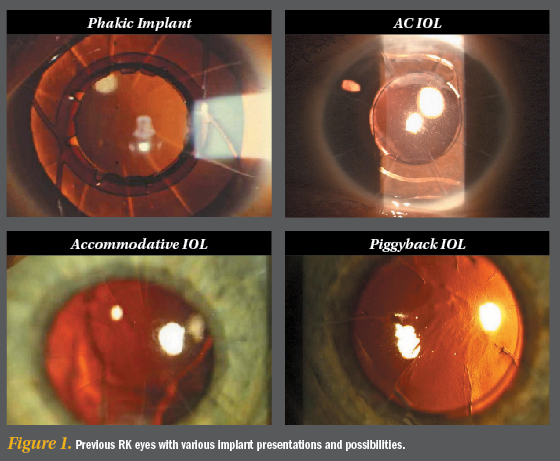
In the second of a two-part series, Arun C. Gulani, MD, reviewed how to address lens-based surgeries when they are associated with previous radial keratotomy.
Ophthalmology Times Editorial Advisory Board Member Jonathan H. Talamo, MD, shared his thoughts on Dr. Gulani's analysis.
“Dr. Gulani astutely deconstructs many of the challenges confronting cataract surgeons in patients with prior RK/AK procedures, offering many valuable pearls to safely navigate the OR and optimize outcomes," Dr. Talamo said. "Incorporating maneuvers such as low flow phaco with manipulation minimized by femtosecond laser pretreatment, prompt management of incision gape or leakage with tissue adhesives such as Resure Sealant or sutures will improve safety and reduce surgeon stress. Optimization of corneal optics with preoperative scar removal, corneal shape/strength using collagen crosslinking, and IOL power selection using intraoperative aberrometry will collectively lead to improved outcomes in this challenging patient population.”
3. Identifying, managing dysphotopsia after cataract surgery
http://ophthalmologytimes.modernmedicine.com/ophthalmologytimes/content/tags/cataract-surgery/identifying-managing-dysphotopsia-after-cataract-su
Earlier this year, we reported how patient symptoms can help physician find anatomic location in optical system.
“Dysphotopsia, especially negative dysphotopsia, remains a troubling phenomenon that plagues otherwise uncomplicated cataract surgery," said Ophthalmology Times Editorial Advisory Board Member Mark Packer, MD. "In the case of negative dysphotopsia, recognized as a dark temporal crescent, consensus has developed around treatment with piggyback IOL implantation (which can also treat any residual spherical refractive error).
"Multifocal dysphotopsia often resolves gradually, while other causes may require a careful refraction and diagnostic testing such as wavefront analysis to determine the cause," he continued. "Time is often on our side in these cases, but IOL repositioning or exchange may ultimately be the best option."
Read how to identify and manage dysphotopsia after cataract surgery