Turning to new frontier in micropulse laser treatment for retinal disorders
Studies show that the micropulse laser represents a safe treatment for macular disorders involving the foveal area. Further and larger studies are needed to prove the real effectiveness related to all the macular pathologies, but it can be used as an add-on to treat complex cases.
The micropulse laser represents a relatively new frontier among retinal specialists. The subthreshold energy it can deliver without damaging retinal tissue is being exploited in various macular diseases, including central serous chorioretinopathy (CSC), diabetic macular oedema (DME), and macular oedema due to branch retinal vein occlusions (BRVO).
There is increasing evidence that subthreshold micropulse laser (SML) treatment (Iridex) can serve as an additional valuable therapeutic option to intravitreal injections (anti-VEGF and/or steroids), mostly for retinal vascular diseases. And, since standardised therapies or established ‘best practice’ guidelines do not yet exist for CSC, the opportunity exists for the micropulse laser to join the armamentarium, particularly in those patients which do not tolerate eplerenone tablets.
In my clinical practice, I am currently using the laser sub-threshold therapy to treat CSC both as monotherapy and in combination with systemic treatments, such as eplerenone or spironolactone.
Principles of action
Conventional laser photocoagulation is widely used to obtain thermal and beneficial effects on the retina; however, it can induce side effects such as chorioretinal atrophy, formation of epiretinal scars, choroidal neovascularisation and visual field defects1.
The SML acts only to stimulate retinal pigment epithelium (RPE) cells to regulate different factors, such as anti-VEGF inhibitors, pigment epithelium-derived factor (PEDF) and permeability factors, sparing the neural retinal and preserving the functional integrity of the photoreceptors2.
Dorin et al.3 delineated well the difference between conventional laser photocoagulation and the micropulse mode. A conventional laser is characterised by the so-called continuous wave (CW) mode, in which the laser energy is delivered with a single pulse, whereas the micropulse mode delivers a train of repetitive short pulses (typically of 100–300 ms), with alternating ‘on’ and ‘off’ times.
The length of time the power is ‘on’ divided by the total time the laser is used gives rise to a ratio known as the ‘duty cycle’. The presence of the so-called ‘off’ time allows the heat to dissipate, thus minimising the thermal effect and reducing retinal injury.
As rigorously covered in recent review by Scholz et al.4, there are currently two different types of micropulse laser. The first is a diode laser with a wavelength of 810 nm, which is able to penetrate up to the choroid.
The other available SML system is the 577-nm yellow laser, which has the advantage that the xanthophyll, a pigment present in the macular layers, absorbs only a minimal amount of yellow light, thereby increasing the safety of a laser procedure close to the fovea. The development of navigated laser systems has considerably improved the accuracy and safety of the micropulse laser treatment. The eye-tracking technology minimises the eye movements of patients, and the presence of special software allows one to plan treatment based on the images obtained with fluorescein angiography (FA) and/or indocyanine angiography (ICG), optical coherence tomography (OCT) and OCT angiography.
In my hospital-based setting, I use the micropulse laser mode with a navigated system and, based on the different macular diseases, I optimise the treatment with the multimodal imaging modality. For example, in the case of CSC, I acquire the FA and ICG images where possible to evidence a typical leakage hot spot, as well as the OCT scan, to demonstrate the presence of subretinal fluid (SRF).
After taking a fundus photo of the patient’s macula, the navigated system is able to superimpose the fundus photo and the OCT/FA/ICG images, and, finally, I can perform the micropulse laser with different energies and duty-cycle at the level of the hot spot evidenced by the FA/ICG and directed to the SRF as illustrated by the OCT scan.
SML treatment in DME
Before the era of anti-VEGF and intravitreal injections, laser photocoagulation was the standard treatment for DME, but severe complications such as accidental foveal damage and expansion of macular scars were observed, and so the method took a back seat.
However, the recent advent of SML has provided a new age for the laser treatment of DME and researchers have sought to assess the safety and efficacy of this therapeutic approach.
One such study5 evaluated functional and morphological parameters after SML treatment with both infrared and yellow systems, showing that the lowest duty cycle (5%) setting seemed to be the safest in order to preserve the visual function and maintain the macular integrity. Moreover, Chhablani et al.6 demonstrated the safety of the two most-used subthreshold parameters (duty cycle 5% and 15%) of the yellow laser compared with conventional laser and found that the 15% duty cycle achieved better anatomical, visual and functional outcomes.
In my routine laser practice, with DME patients, I usually set the duty cycle to 10% with a power energy between 120 and 160 mW, associated with the laser-navigated treatment mode. So far, I have not had any cases of choroidal neovascularisation, photoreceptor integrity damage or laser-related visual function deterioration, which I believe demonstrates how safe the micropulse procedure is.
Macular oedema due to BRVO
Another interesting field is the application of the micropulse laser for the treatment of patients with macular oedema (MO) following an episode of BRVO. As recently summarised in a review by Eng et al.7, SML appears to be safer than conventional laser photocoagulation and is as efficacious, improving visual function and reducing the intraretinal fluid accumulation in such patients.
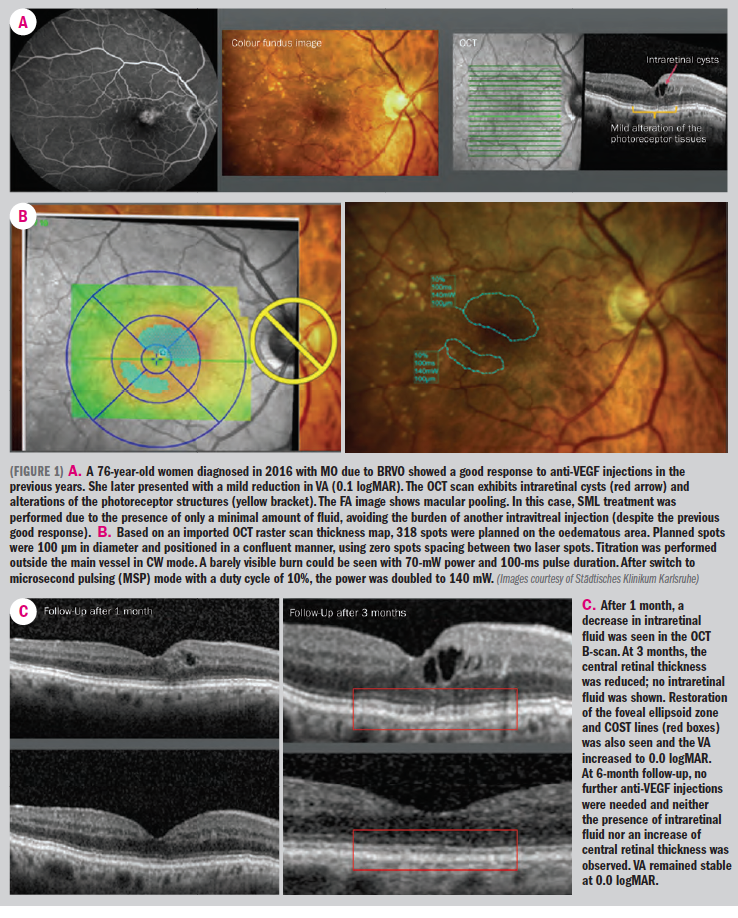
In a small retrospective series presented by our team at the European Society of Retina Specialists (EURETINA) congress, we analysed the safety and efficacy of the yellow navigated micropulse laser treatment in 17 patients (18 eyes) affected by MO due to BRVO with a follow-up of 3 months. We observed a statistically significant improvement of the visual acuity without a corresponding decrease in macular thickness.
Interestingly, we found that the photoreceptor structures were restored, particularly in terms of renewal of the ellipsoid zone integrity. Moreover, confirming the previous data regarding the safety of the procedure, we saw no cases of chorioretinal atrophy, scarring or choroidal neovascularisation. We had set the duty cycle to 10% and used 130 mW as medium energy with circa 600 spots at the level of the increased macular thickness (see Figure 1A–C).
Combining the micropulse laser with intravitreal injections can help to reduce the burden of numerous injections. In a recent study, Terashima et al.8 determined the efficacy and safety of the combination therapy between the yellow SML and intravitreal ranibizumab, showing that visual acuity was maintained with a decreased number of intravitreal procedures needed.
I agree with this treatment modality and in my practice I tend to combine the intravitreal approach (anti-VEGF and steroid implants) with the micropulse laser to tackle the disease in different ways, and so reduce patients’ stress and achieve the best functional result.
Central serous chorioretinopathy
The standardised treatment for CSC has been the subject of debate due to the lack of data from randomised controlled trials. The first pilot study to investigate the role of micropulse laser treatment for CSC was presented in 20039. The SML (with 810-nm diode laser) led to the complete resorption of SRF 1 month after the treatment with no recurrence at 6-month follow-up.
Since 2003, many different studies have analysed the efficacy of the micropulse laser for chronic CSC, with encouraging results. Nevertheless, the PLACE trial10, an open-label, multicentre, randomised, controlled clinical study, recently demonstrated that a significantly higher proportion of patients receiving half-dose photodynamic therapy (PDT) achieved complete resolution of SRF and functional improvement than those subjected to high-density SML (HSML).
However, in the literature there are other interesting studies which prove the efficacy of the micropulse laser for cases of CSC.
For example, Kim et al.11 conducted a retrospective study with a 3-year follow-up demonstrating a complete SRF reabsorption in 81.5% of patients affected by chronic CSC who were treated with yellow 577-nm SML.
Unlike the other published studies, which used a conventional treatment duration of 100–300 ms, the research group opted for just 20 ms, with a 15% duty cycle and a power ranging from 200 to 400 mW, applying the energy both over the area of RPE leakage and all areas of serous retinal detachment, including the fovea.
In my clinic, I follow the indications of the previous study, but slightly modifying the parameters: for the leakage point assessed by multimodal imaging modality (FA/ICG), when it is located far away from the foveal zone, I use a 15% duty cycle, 20-ms treatment duration and 300 mW of energy; whereas, for the SRF, mostly if it is localised at the foveal level, I usually use a 10% duty cycle, 20-ms duration and 150-mW energy, in order to stimulate only the RPE cells, avoiding damage to the foveal area.
Conclusions
Studies show that the micropulse laser represents a safe treatment for macular disorders involving the foveal area. Regarding the efficacy, the results are not still uniform and for this reason we need further and larger studies to prove the real effectiveness related to all the macular pathologies.
In my opinion, we can currently consider the micropulse laser as an additional therapy, which may help physicians to treat disorders with complex pathophysiology, such as DME, MO due to BRVO, and CSC. The feasibility of using the micropulse laser in combination with intravitreal injections in the case of MO related to vascular disorders offers the potential to relieve the burden of injections, help with patient compliance and optimise functional outcomes.
In the case of CSC, the laser acts as another therapeutic option besides PDT with minimal risks and good efficacy, both as monotherapy and when associated with other treatment strategies, such as eplerenone and spirinolactone.
Disclosures:
EMILIANO DI CARLO, MD
E: emi.dicarlo@hotmail.it
Dr Di Carlo is a vitreoretinal consultant at the ophthalmology department of the Städtisches Klinikum Karlsruhe, Germany. His main interests are micropulse laser and new frontiers of vitreoretinal surgery. He has no financial interests in the subject matter.
CAMILLA SIMINI, MD
E: camilla.9128@gmail.com
Dr Simini is an ophthalmology resident at Städtisches Klinikum Karlsruhe, Germany, which is directed by Prof. A.J. Augustin. Her main interests are: medical and surgical retina. She has no financial disclosures.
References:
1. Seiberth V, Alexandridis E, Feng W. Function of the diabetic retina after panretinal argon laser coagulation. Graefes Arch Clin Exp Ophthalmol. 1987;225(6):385-390.
2. Ulbig MR, Arden GB, Hamilton AP. Color contrast sensitivity and pattern electroretinographic findings after diode and argon laser photocoagulation in diabetic retinopathy. Am J Ophthalmol. 1994;117(5):583-588.
3. Dorin G. Evolution of retinal laser therapy: minimum intensity photocoagulation (MIP). Can the laser heal the retina without harming it? Semin Ophthalmol. 2004;19:62-68.
4. Scholz P, Altay L, Fauser S. A Review of Subthreshold Micropulse Laser for Treatment of Macular Disorders. Adv. 2017;34:1528-1555.
5. Vujosevic S, Martini F, Longhin E, Convento E, Cavarzeran F. Subthresold micropulse yellow laser versus subthresold micropulse infrared laser in center-involving diabetic macular: Morphologic and Functional Safety. Retina. 2015;35:1594-1603.
6. Chhablani J , Alshareef R , Kim DT, Narayanan R, Goud A et al. Comparison of different settings for yellow subthreshold laser treatment in diabetic macular edema. BMC Ophthalmol. 2018;18:168.
7. Eng VA, Leng T. subthreshold laser therapy for macular oedema from branch retinal vein occlusion: focused review. Br J Ophthalmol. 2020 Feb 7 [Online ahead of print].
8. Terashima H, Hasebe H, Okamoto F, Matsuoka N, Sato Y et al. Combination therapy of intravitreal ranibizumab and subthreshold micropulse photocoagulation for macular edema secondary to branch retinal vein occulsion: 6 month result. Retina. 2019;39:1377-1384.
9. Bandello F, Lanzetta P, Furlan F, Polito A. Non-visible subthreshold micropulse diode laser treatment of idiopathic central serous chorioretinopathy. A pilot study. Investig Ophtalmol Vis Sci. 2003;44:4858.
10. van Dijk EHC, Fauser S, Breukink MB, Blanco-Garavito R, Groenewoud JMM et al. Half-dose photodynamic therapy versus high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy: the PLACE trial. Ophthalmology. 2018;125:1547-1555.
11. Kim YJ, Kim SY, Ha S, Moon D, Seong S et al. Short-duration multiple-session subthreshold micropulse yellow laser (577 nm) for chronic central serous chorioretinopathy: results at 3 years. Eye (Lond). 2019;33:819-825.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.