Ultra-widefield FA vital for recalcitrant DME
Ultra-widefield fluorescein angiography may help improve treatment in patients with recalcitrant diabetic macular edema by visualizing areas of peripheral nonperfusion that can benefit from targeted photocoagulation.
Take-Home:
Ultra-widefield fluorescein angiography may help improve treatment in patients with recalcitrant diabetic macular edema by visualizing areas of peripheral nonperfusion that can benefit from targeted photocoagulation.
Dr. Patel
By Lynda Charters; Reviewed by Seenu M. Hariprasad, MD and Ravi D. Patel, MD
Chicago-A new technology has found that patients with large areas of retinal nonperfusion and severe diabetic retinopathy (DR) seem to have the most diffuse recalcitrant diabetic macular edema (DME), said Ravi D. Patel, MD.
The new technology-ultra-widefield fluorescein angiography (FA)-allows the simultaneous visualization of peripheral retinas more than what was previously achievable, said Dr. Patel, associate vitreoretinal surgeon and director of clinical research at Retinal Vitreal Consultants Ltd. in Chicago.
To determine this finding, Dr. Patel and his colleagues conducted a retrospective, observational case series of patients with recalcitrant DME for a minimal period of 2 years.
The study
The charts of 1,156 patients with type 2 diabetes mellitus diagnosed from Sept. 2, 2010 to March 30, 2012 were reviewed, of whom 76 patients (148 eyes) were being treated and met the inclusion criteria.
All patients underwent ultra-widefield FA with an imaging system (C200 MA, Optos) and optical coherence tomography (Cirrus, Carl Zeiss Meditec Inc.) on day 1 of the study.
Before the ultra-widefield FA images were obtained, patients received a standard intravenous infusion of sodium fluorescein. The macular thickness was measured on spectral domain (SD)-OCT images.
The mean outcome measures were the mean ischemic index, mean change in the central macular thickness (CMT), and the mean number of focal photocoagulation treatments applied to the macula over the course of the 2-year study.
The patients with recalcitrant DME were divided into 4 cohorts based on the severity of their DR:
· Mild nonproliferative DR (NPDR)
· Moderate NPDR
· Severe NPDR
· Quiescent proliferative DR (PDR) after panretinal photocoagulation (PRP)
The mean overall ischemic index in all patients was 47%, Dr. Patel said. The mean ischemic indexes based on the severity of the DR were 0%, 34%, 53%, and 65%, respectively.
The mean respective decreases in CMT values were 25.2%, 19.1%, 11.6%, and 7.2%, and the mean number of application of focal photocoagulation were 2.3, 4.8, 5.3, and 5.7.
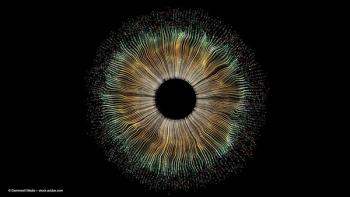
Ultra-widefield fluorescein angiography provides a more extensive visualization of peripheral retina for more focused treatment of recalcitrant diabetic macular edema. (Image courtesy of Ravi D. Patel, MD)
Disseminating the results
Dr. Patel said he found that the retinal vascular nonperfusion that is untreated might be associated with recalcitrant DME. In the study, 80% of patients with recalcitrant DME had evidence of untreated nonperfusion.
“Calculating the ischemic index allowed us to quantify nonperfusion and place a ratio of nonperfused to perfused retina,” he said. “Our results demonstrate that the most recalcitrant DME existed in patients with the largest areas of retinal nonperfusion . . . (and) as a result, these patients had the least amount of reduction in the CMT, requiring the greatest amount of macular photocoagulation treatments.”
Dr. Patel underscored the role of ultra-widefield FA in visualizing the pathology in the peripheral retina in patients with DR, and said he believed that detection and delineation of areas of retinal vascular nonperfusion may be clinically valuable.
“The association between retinal capillary nonperfusion and recalcitrant DME found in this study supports the hypothesis that zone of untreated retinal nonperfusion may stimulate production of biochemical mediators leading to recalcitrant DME and a suboptimal response to therapeutic treatments,” he said. “Therefore, ultra-widefield FA may be a valuable tool to identify therapeutic target areas for photocoagulation, allowing for efficient treatment of ischemic retina and potentially decreasing the production of vascular endothelial growth factor and cytokines that play a role in recalcitrant DME.”
Ravi D. Patel, MD
E: raviretina@gmail.com
Dr. Patel has no financial interest in the subject matter.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.