World Retina Day: New data from Kiora Pharmaceuticals shines a light on inherited retinal diseases
Kiora CEO Brian Strem, PhD, offers an update on the development of KIO-301, a molecule that selectively targets retinal ganglion cells, giving them the ability to sense light.
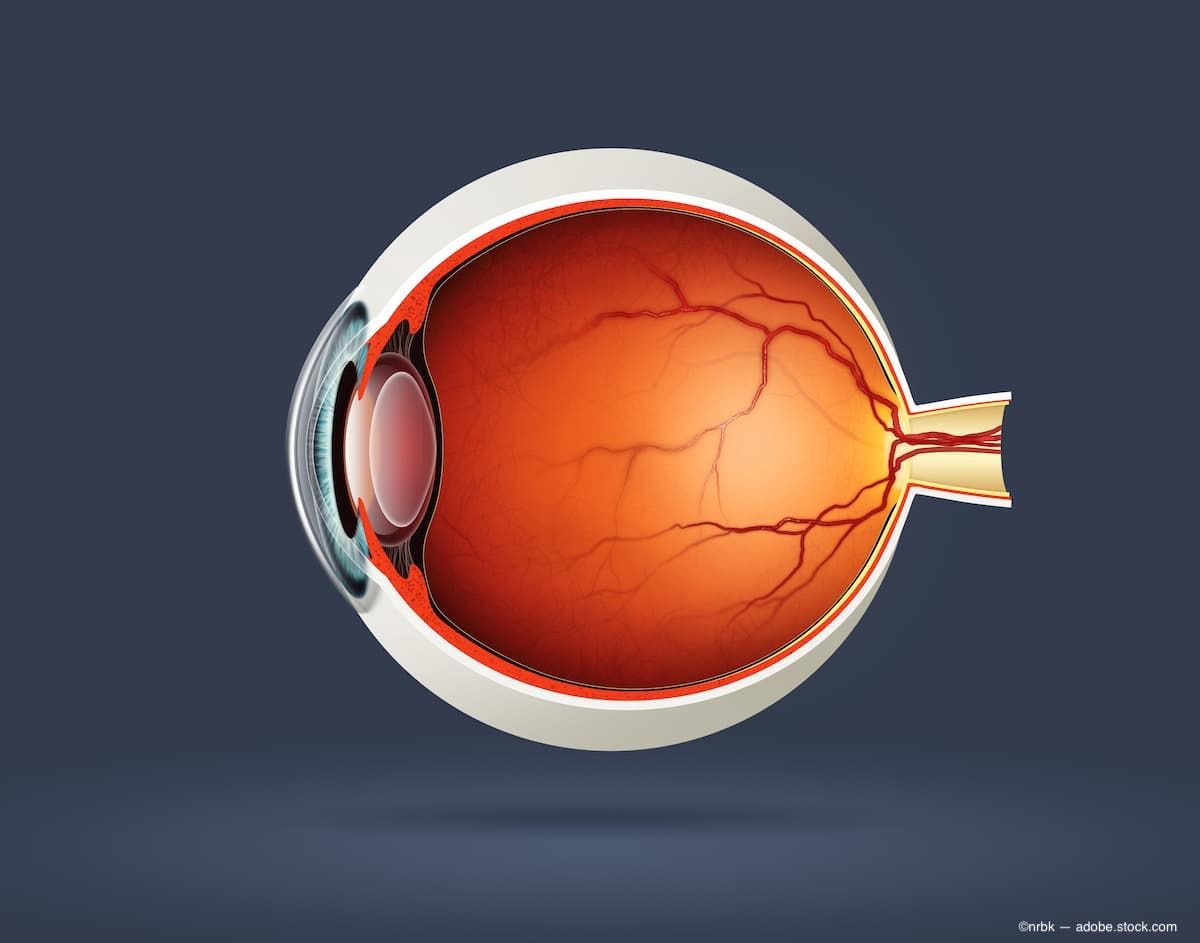
(Image Credit: ©nrbk - Adobe.Stock.com)
Set against the backdrop of World Retina Day on Sept. 24 and Vision Awareness Month in October, ophthalmologists continue to look for new treatment options to help preserve the vision of patients, including more than 2 million people worldwide who are facing a loss of eyesight due to an inherited retinal disease.
In a conversation with Ophthalmology Times, Brian Strem, PhD, CEO of Kiora Pharmaceuticals, discussed the challenges patients diagnosed with an inherited retinal disease (IRD) face as well as data on the development of KIO-301, a molecule that selectively targets specialized neurons called retinal ganglion cells (RGCs), giving them the ability to sense light.
KIO-301 is a visible light-sensitive small molecule that acts as a reversible 'photoswitch', specifically designed to restore the eyes' ability to perceive and interpret light in visually impaired patients. KIO-301 selectively enters retinal ganglion cells (those downstream of degenerated rods and cones) and 'switches' them into light sensing cells, capable of signaling the brain as to the presence or absence of visible light.
The range of IRDs include more than 20 or so diseases that have been well defined, according to Strem, with more being discovered each day.
“We know that these can be caused by more than 250 different known gene mutations that are just inherited,” he said. “So, you get it. You have it at birth. And unfortunately, that means it's, it's going to lead to a disease that's going to take you down the loss of vision pathway.”
Globally, from 2 million to 4 million patients are impacted by IRDs, Strem noted, with some diseases proving to be more severe than others. There are limited options for ophthalmologists who are treating these patients, and often the only recourse can be to minimize the loss of vision.
The impact of the care of patients with IRDs can prove to be a financial hit, Strem noted, with an estimated $13 billion to $32 billion spent in the US alone each year.
“So it's, it's a pretty substantial impact to the health care costs that we have here,” he explained. “Again, with really very little therapeutic options for these patients.”
Retinitis pigmentosa remains one of the most prevalent IRDs, and it comprises a group of diseases that all present in a similar fashion, though Strem noted it can manifest at varying times in a patient’s life and at varying rates of progression.
“For some, it could be more severe diseases like x-linked RP, that will include patients in their 30s who are completely blind or who have no light perception,” he noted. “Whereas some of the other forms of RP will have some form of vision, with patients whose vision will be very bad and likely they will be legally blind before they go fully blind in their kind of 70s and 80s.”
This leaves retina specialists on the front lines of treatment of these diseases, and Strem pointed out that there are new developments daily in the development of therapeutics to preserve the vision of these patients.
“There are a lot of groups like us who are dedicated to trying to help these patients,” he pointed out. “Retinal specialists are attending the conferences, but they can take advantage of industry days that precede those conferences … things like the Eyecelerator Conference or the OIS conference. These are great way is where a lot of industry comes together, along with a lot of the key opinion leaders. And even more on the finance, banking, investor side, everyone kind of gets together for a day and highlight some of the key advancements in this space.”
During the Retinal Subspecialty Day at the American Academy of Ophthalmology 2023 annual meeting in San Francisco, Kiora will present data from an ongoing clinical trial showing KIO-301 has the potential to restore light perception in patients who are blind or living with ultra-low vision due to retinitis pigmentosa.
The trial, called the ABACUS study, is a Phase 1b open-label, single ascending dose clinical trial for people living with retinitis pigmentosa. The study comprises the enrollment of six patients and the evaluation of 12 eyes, following monitoring for 29 days. The first cohort of three patients includes individuals with no or bare light perception due to the progression of RP. The second cohort includes three patients able to detect hand motion and count fingers. The primary endpoints are safety and tolerability, with secondary efficacy endpoints including object identification and contrast assessment, navigation, fMRI and other ophthalmic and quality-of-life assessments.
“This is an incredibly novel small molecule that was actually discovered out of UC Berkeley, where it's a light responsive molecule, which means when light touches the molecule, it actually changes shape,” Strem explained. “And with the rest of the molecule, it was designed to actually go in specifically to these neurons that make up the optic nerve in the brain in the eye. And it converts them into actually being light sensitive.”
Stem noted that the molecule is bypassing the normal light sensitive cells in the red, which are the rods and the cones, we all know as photoreceptors, and is creating an ability to detect light to these retinal ganglion cells.
“In the case of these inherited retinal diseases, like RP, we know those patients have degenerated or dead photoreceptors,” he said. “So, even if you're trying to target those with gene therapies or other approaches, they're not there. They're not viable anymore. So we have to find alternative solutions to give vision back to these patients.”
This research could ultimately lead to a therapeutic option for retina specialists to turn to for the patients they treat with these inherited retinal diseases.
“We believe that this is a tool that they can hopefully put in their bag with patients who have later stage disease, where there's already dead sections of the retina, if you will, or the photoreceptors, and then give them the ability to restore some of that functional vision,” Strem said. “What's important is, does it actually improve a patient's ability to do things like navigate, and improve their quality of life.
Strem noted that it isn’t possible to take a patient who is totally blind and restore their vision to the point that they can read a normal book. He said that would be asking too much.
“We take that patient, and let them be able to walk into a bank and find the teller stand without needing assistance or without needing the help of a guide dog or asking other individuals to guide them towards where they need to go,” he said. “It is that type of benefit that our drug could potentially be able to actually give these patients back.”
Kiora recently completed its first-in-human Phase 1b clinical trial of KIO-301, which was tested in 6 patients, to demonstrate its safety.
“We also are assessing the ability of the drug to actually give some of this vision back and whether that is the functional vision, whether it's improving what's called visual acuity,” he said.
This includes determining how patients are seeing in their central vison and whether visual fiends can be expanded to include improvements to peripheral vision as well.
“The idea is to take this into the next phase of studies, where we're going to be doing a multi-dose study,” Strem said. “We are going to be treating these patients about once a month for the course of 3 to 6 months. We will then continue to assess patients to see if it continues to benefit patients as was seen in the first single-injection study.”
World Sight Day and Vision Awareness Month increase awareness of these issues, including IRDs, but the work being conducted by companies worldwide is providing hope for those people who facing a life of limited vision or even darkness.
“We all rely so heavily on vision in our normal day to day,” Strem said, pointing out that many patients often get to the point where they just give up. “That tells me that we're failing as a medical community. We need to be doing something better to actually not let these patients lose their hope, towards being able to either slow the progression of their vision loss, or restore what was already taken from them.”
That proves to be a motivator for Strem, and of Kiora Pharmaceuticals also has another asset, dubbed KIO-104 in its pipeline, which he described as a small molecule, non-steroidal anti-inflammatory drug.
“It's a novel mechanism of action that's being used in diseases like multiple sclerosis and rheumatoid arthritis,” he said. “We have a molecule that can target the same pathways and knock down the inflammatory response in the eye. And so that study or that program right now is focused on an orphan disease as well called posterior non-infectious uveitis. We've already done a little bit of clinical work there, and honestly are looking for a partner to help us advance that program forward.”