Case #2: A 52-year-old With Recurrent Uveitis
Thomas Albini MD reviews the case of a 54-year-old male with chronic non-infectious uveitis.
Thomas Albini, MD: The second case I wanted to share with you today is a case of episodic blurry vision in both eyes. This is a 54-year-old man I met long ago, referred by a retina specialist for what was thought to be multifocal choroiditis. He had visual problems that had occurred 1 week prior and lasted for 10 minutes. He was also complaining of photophobia, and he had a history of hypertension, prostate cancer, chronic anxiety, fibromyalgia. At the time, he was on oral prednisone that had been started by the retina specialist; Xanax, Percocet, and the other medicines.
He had 20/40 vision in the right eye, 20/20 in the left eye. Pressure was a little bit more elevated in the right than in the left. No cells were seen in the anterior chamber and clear lenses. These are fairly old fundus photos, but you see there that he has a number of these creamy yellow lesions, particularly in the inferior nasal quadrant. This is the right eye. On the right-hand side, you see the nasal portion of the right fundus, with those multiple creamy lesions surrounding the optic nerve most prominently in the nasal quadrant. In the left eye, he has very similar lesions with the very symmetric distribution. You see on the infrared image here that those lesions light up. Fluorescein angiogram shows that most of the lesions are not seen or appreciated on the fluorescein angiogram, although there are some window defects suggesting some atrophy. There were similar findings for the left eye. Some blood tests were obtained, and my clinical suspicion was for birdshot chorioretinopathy. This patient did have mild uveitis, very symmetric bilateral disease and presented in his 50s. I obtained an HLA 829 which was positive and went along with that diagnosis. A diagnosis of birdshot chorioretinopathy was made.
I treated the patient with a number of different off-label immunosuppressive medicines. He failed cyclosporine treatment. We started azathioprine 50 mg twice a day. CellCept was not something that was covered by his insurance, and, in those days, was still a more expensive drug. Methotrexate and azathioprine were more economical, but he felt that all of these drugs made him feel very fatigued and he did not like taking them. He was very honest about the fact that he was not going to continue to take them in spite of some benefit that was seen with his vision.
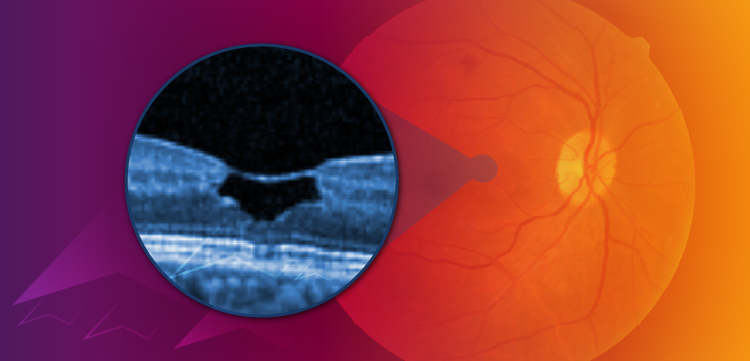
One year later, these are montage fundus photos, and you see those radial creamy lesions that, along with the HLA typing of 829, make the diagnosis of birdshot. He's still unhappy with his systemic immunosuppression, although his vision has improved to some degree. Finally, after discussing with the patient, we decided to put in bilateral surgically implanted fluocinolone implants. He tolerated the procedure very well. His visual acuity improved in both eyes, was subjectively better, and actually showed stable Humphrey visual fields and improved ERGs in both eyes after the implants had been in for some time. He remained quite well controlled on these. He'd undergone registered exchanges subsequently and his vision continued to improve. ERGs got better and the vision had improved to 20/20 and 20/25. He did ultimately need cataract surgery and glaucoma surgery, as tubes in both eyes as is very common with the registered implant virtually. Every patient with the surgically placed registered implant will need cataract surgery in the first year of use and about a third of the patients are going to need glaucoma surgery. Overall, the surgeries went well, and he had great vision and was very happy with the treatment strategy. He did require an Ozurdex injection due to breakthrough inflammation, with some cystoid macular edema, and, unfortunately, suffered endophthalmitis following that injection; it's the only endophthalmitis following injection I've been unfortunate enough to experience. He has not bounced back. His vision has remained poor. I've been very concerned about further surgical intervention on his left eye now, which is 20/20 eye. And instead replacing the Retisert with a new one, I have opted to treat him with Yutiq in both his eyes and he's done very well with Yutiq placement instead of repeat surgery for Retisert and has remained quiet and well-controlled with the injectable fluocinolone implant. In this functionally one-eye patient, that was a better choice to make sure we preserve the vision that he has there.
Transcript Edited for Clarity
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.