- Modern Retina Fall 2022
- Volume 2
- Issue 3
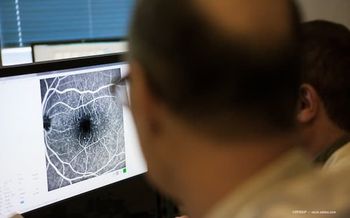
Increased dosing for treatment of X-linked retinoschisis linked with inflammation in AAV-RS1 trials
Investigators have reported good progress in determining how the disease works in the eye; however, a downside is the inflammation that seems to accompany treatment with increased dosing.
X-linked retinoschisis (XLRS) is a congenital disorder that results in visual impairment in boys at an early age. No treatment is currently available, and surgical repair fails in many cases. Retinal damage in the periphery includes tears and retinal surface bubbling, scarring, and fibrosis.
XLRS affects the retina both structurally and functionally, ie, splitting of the retinal layers across the macula and periphery and cysts present; an increased risk for hemorrhage and detachment; and on electroretinography (ERG), interrupted transmission from the a-wave to the b-waves (from the rods to the bipolar cells) and reduced or lost ERG b-wave. The RS1 protein is localized to the rod inner segment and the outer plexiform layer synapses.
Investigators have reported good progress in determining how the disease works in the eye; however, a downside is the inflammation that seems to accompany treatment with increased dosing. Paul Sieving, MD, PhD, described recent study outcomes and focused on the inflammatory component associated with treatment. Sieving is the Neil and MJ Kelly Presidential Chair and director of the Center for Ocular Regenerative Therapy at University of California, Davis in Sacramento.
XLRS research
The XLRS protein is not exclusive to the eye, according to Sieving, and is found in the lung as well.1 Other authors suggested the role of the protein in lung carcinoma; they found that in lung adenocarcinoma, the prognosis is worse if the tissue has low expression of RS1 protein, indicating that the protein may be seen by the systemic circulation,2 Sieving explained.
Regarding the protein localization, investigators reported that an element of the synapses, the trip channel (conductance channel), was found to be missing in RS1 knockout retinas in mice, which impairs signaling of the synapses to the bipolar cells.3 After therapy, in a normal retina, the molecules of the signaling cascade are tightly localized to the dendritic tips; in contrast, in the knockout model, the molecules are delocalized along the shaft of the dendrites.
In Sieving’s laboratory where they constructed a knockout transgenic mouse model that replicated human disease, ERG images showed the presence of the a-wave and the absence of the b-wave.
The investigators then created a vector to treat this scenario and injected it into the middle of the vitreous. They found RS1 protein expression in the wild-type mouse retina and in the adeno-associated vector (AAV)-RS1 vector-treated retinas, in which the RS1 expression was restored and the schisis cavities were absent; however, the untreated knockout retina showed schisis cavities and no RS1 expression, Sieving reported.
Likewise, the retinal structure was restored after the vector treatment, and the b-wave recovered.
The next step in Sieving’s research involved testing the vector injected into the vitreous in a human phase 1/2a clinical trial.4 Four doses were tested (1e9-3e11) in 12 patients. He reported one particular patient of interest who had cavities before dosing, but the cavities were sealed shut by 14 days after dosing. “We are viewing this result as some evidence of biologic activity,” he commented.
Inflammation development
The first 2 lower doses in the phase 1/2a study were not associated with inflammation. Last-onset inflammation developed in 1 patient who received dose 1e10 that resolved with oral steroid therapy; another patient had preexisting neutralizing antibody and had a very strong antibody response that was maintained without signs of clinical inflammation.
Three patients on the highest dose had varying degrees of ocular inflammation; pretreatment with a steroid was not administered to 2 patients but was administered to the third patient, who despite the pretreatment developed “considerable” inflammation, but the cavities closed. “This means that ocular inflammation cannot always be averted despite predosing with steroids,” Sieving said.
The next step was a return to the mouse model to study the retina transcriptome at baseline and after dosing. The findings were interesting because a young mouse had many upregulated genes associated with immune system processes. “This indicated that there is preexisting immune activation in the retinas with retinoschisis,” he pointed out.
After vector treatment, the upregulation was moderated, and wound-healing genes were upregulated with movement toward a recovery phase.
Baseline inflammatory contribution
This raised the question about whether baseline inflammatory disease contributes to a vector immune response.
An investigation5 into serum samples from 11 human patients dosed with the vector showed serum markers before vector dosing, ie, CD4+ T cells were upregulated, and CD8+ T cells were downregulated. The ratio of the 2 cell types was increased at baseline and represents a marker of immune activation.
Again, a question arose about whether baseline inflammation from retinal degeneration causes a pro-inflammatory response to the AAV vector.
Sieving reported that the degree of inflammation after vector treatment in these patients was correlated roughly with the baseline CD4+/CD8+ cell level. In addition, cytokines and interferon-γ levels also were upregulated after vector treatment, which was unexpected because these are systemic immune markers.
Based on this small study, Sieving had the following takeaways:
- Patients who received the same vector doses showed considerable variability in response and inflammation.
- Pretreatment with a steroid did not abrogate the immune response.
- Pretreating with immune suppression appeared to reduce the immune response and inflammation in 1 of 2 patients.
- The highest dose of the vector provided preliminary signs of retinal biologic activity.
A question for future research is the immune baseline status and how an ocular disease is reflected in the blood/plasma compartment.
Paul Sieving, MD, PhD
E: pasieving@ucdavis.edu
This article is adapted from Sieving’s presentation at the American Society of Gene and Cell Therapy 25th Annual Meeting in Washington, DC. He is a cofounder of VegaVect, Inc and Avista Therapeutics and on the scientific advisory boards of SparingVision and the Institute of Molecular and Clinical Ophthalmology Basel.
References
1. Tolun G, Vijayasarathy C, Huang R, et al. Paired octamer rings of retinoschisin suggest a junctional model for cell-cell adhesion in the retina. Proc Natl Acad Sci U S A. 2016;113(19):5287-5292. doi:10.1073/pnas.1519048113
2. Zhang T, Cheng G, Chen P, et al. RS1 gene is a novel prognostic biomarker for lung adenocarcinoma. Thorac Cancer. 2022;13(12):1850-1861. doi:10.1111/1759-7714.14471
3. Ou J, Vijayasarathy C, Ziccardi L, et al. Synaptic pathology and therapeutic repair in adult retinoschisis mouse by AAV-RS1 transfer. J Clin Invest 2015;125(7):2891-2903. doi:10.1172/JCI81380
4. Cukras C, Wiley HE, Jeffrey BG, et al. Retinal AAV8-RS1 gene therapy for X-linked retinoschisis: initial findings from a phase I/IIa trial by intravitreal delivery. Mol Ther. 2018;26(9):2282-2294. doi:10.1016/j.ymthe.2018.05.025
5. Mishra A, Vijayasarathy C, Cukras CA, et al. Immune function in X-linked retinoschisis subjects in an AAV8-RS1 phase I/IIa gene therapy trial. Mol Ther. 2021;29(6):2030-2040. doi:10.1016/j.ymthe.2021.02.013
Articles in this issue
over 3 years ago
Expanding our vision of steroid-eluting implantsover 3 years ago
Acing the suprachoroidal injection for targeted drug deliveryNewsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.