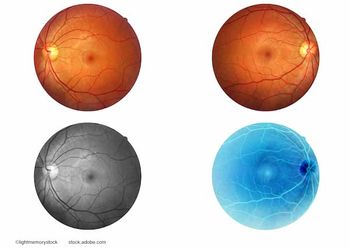
Mapping the specific progressing anatomic features from drusen to type 3 MNV
Elodie Bousquet, MD, PhD, and international researchers studied type 3 macular neovascularization (T3 MNV) using optical coherence tomography. In 64.5% of 31 eyes with T3 MNV, it developed over soft drusen, showing drusen growth and outer layer thinning before T3 MNV.
Recognition of the changing anatomic face of
Bousquet is from the Retinal Disorders and Ophthalmic Genetics Division, Stein Eye Institute, University of California Los Angeles, David Geffen School of Medicine at UCLA, Los Angeles, and the Department of Ophthalmology, University of Paris Cité, Lariboisière Hospital, Assistance Publique-Hôpitaux de Paris, Paris.
The researchers used tracked spectral-domain
The OCT parameters that were assessed were the height and width of the drusen, outer nuclear layer/Henle fiber layer thickness at the drusen apex, and the presence of intraretinal hyperreflective foci, disrupted retinal pigment epithelium (RPE), incomplete RPE and outer retina atrophy, and complete RPE and outer retina atrophy.
Thirty-one eyes with T3 MNV were included in the study.
In almost two-thirds of the eyes, 64.5% (n=20 eyes), the T3 lesions developed over the soft drusen. The drusen showed progressive growth (P < 0.001) that was associated with outer nuclear layer/Henle fiber (P < 0.001) thinning before the development of T3 MNV, the authors reported.
They identified the following features on the OCT images that preceded the development of T3 MNV, ie, disruption of the external limiting membrane/ellipsoid zone and/or the RPE, hyperreflective foci, and incomplete RPE and outer retina atrophy/complete RPE and outer retina atrophy. T3 MNV was seen typically at the apex of the drusenoid lesions.
The major finding was that specific anatomic changes preceded the development of T3 MNV that most commonly originated above the soft drusen. The changes included drusen growth, reduced outer nuclear layer/Henle fiber thickness, and RPE atrophy at the drusen apex.
The authors commented, “Identifying these OCT features should warrant close monitoring for identification of T3 MNV, which can benefit from prompt intravitreal anti-vascular endothelial growth factor therapy.”
Reference:
Bousquet E, Santina A, Corradetti G, et al. From drusen to type 3 macular neovascularization. Retina. 2024;44:189-196; doi:10.1097/IAE.0000000000003945
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.