New dawn of GA management requires renewed attention to imaging
It is important that the ophthalmic community redouble our efforts in following patients with age-related macular degeneration (AMD) using optical coherence tomography (OCT) to find the early signs of geographic atrophy (GA).
The landscape of geographic atrophy (GA) management has changed dramatically. For the first time, we have treatment options with the approval of 2 pharmaceuticals, pegcetacoplan injection (Syfovre; Apellis Pharmaceuticals) and avacincaptad pegol intravitreal injection (Izervay;
Iveric Bio). In light of these advancements, it is important that we in the ophthalmic community redouble our efforts in following patients with age-related macular degeneration (AMD) using optical coherence tomography (OCT) to find the early signs of geographic atrophy (GA).
Patient to watch
There are 3 groups of patients whom eye care providers should monitor to identify as immediate or potential candidates for GA treatment. They should be educated about the new treatment options to understand that it is crucial they keep their follow-up exam schedule.
The first group includes symptomatic patients who already have lesions that are affecting vision. These individuals commonly report having difficulty with contrast sensitivity and seeing at night and may report that when looking at a word not all the letters are visible. The exam will show macular atrophy, and consideration should be given to starting treatment promptly. Clinical trial data have demonstrated that the longer patients receive treatment, the greater the treatment benefit, compared with observation.
The second group includes patients with macular lesions who are not yet candidates for treatment with the new agents but will have progression to GA. They should be encouraged by their primary eye care provider to have regular follow-ups and perhaps be referred to a retina specialist for monitoring. OCT imaging will reveal drusen with hyper-reflective foci; some drusen may show the beginning of hypertransmission. Within a year, these patients may begin to have signs of GA.
Patients with nascent GA make up the third group. They typically have a wedge defect in the retinal nerve fiber layer as well as subsidence of the inner nuclear layer and outer plexiform layer. They are likely to progress to GA and should likewise be closely followed, and treatment initiated once appropriate.
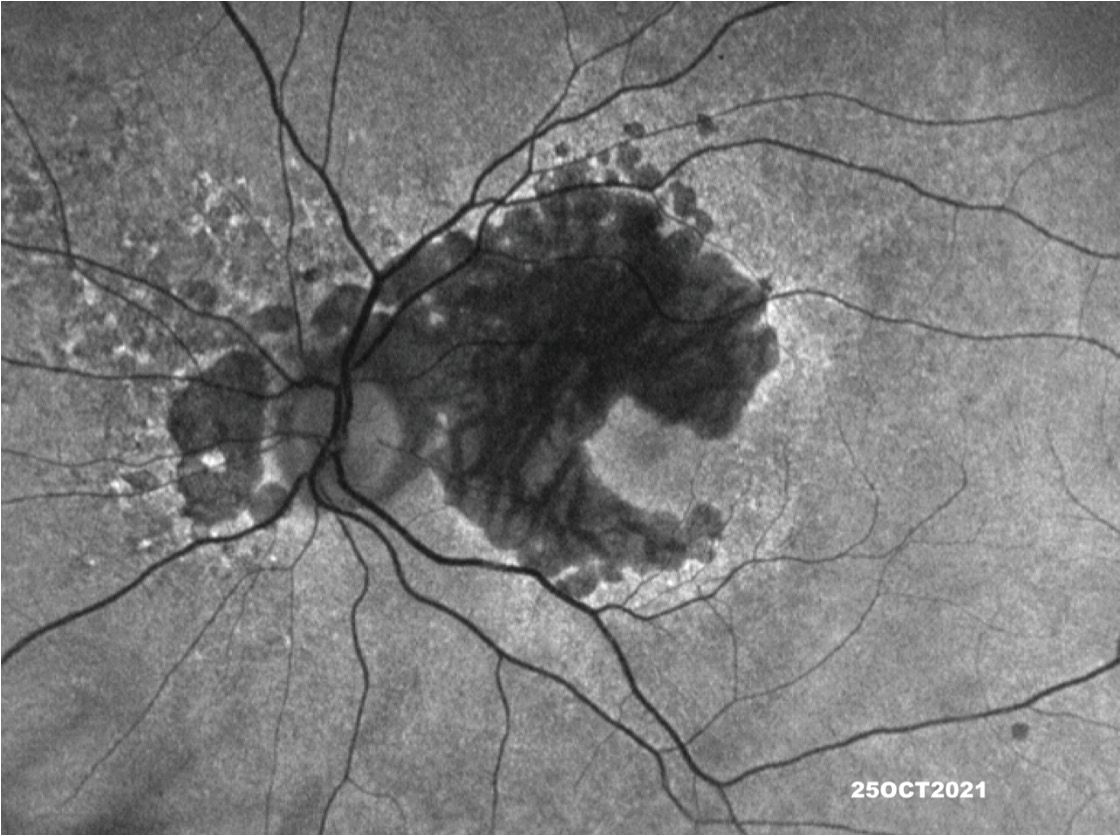
Figure 1.
(Image courtesy of Jeremiah Brown Jr, MD)

How to spot GA
An OCT B-scan provides a cross-sectional view of the retina. Atrophy can be seen with the en face view using the platform’s near-infrared light as well as on autofluorescence imaging. For example, with multimodal SPECTRALIS OCT (Heidelberg Engineering), I can obtain an image before I
administer fluorescein, revealing fluorescence of the retinal pigment epithelium (RPE) layer. Areas of atrophy will be outlined by gaps that show less fluorescence or hypo-autofluorescence. (Figure 1) Today, many providers use widefield imaging systems. These devices also offer an autofluorescence mode for identification of atrophy.
Of note, the new drugs are approved specifically for patients who have GA due to AMD. They are not indicated for use in patients who have atrophy from an inflammatory macular scar, monogenic hereditary retinal diseases, or old neovascularization scarring that resulted in an RPE tear. These patients were not included in the drug trials; more research is needed to understand the benefits of treatment in other populations.
Figure 2. Hyperautofluorescent retinal pigment epithelium cells along the border of the geographic atrophy.
(Image courtesy of Jeremiah Brown Jr, MD)
In true GA due to AMD, the RPE cells will be autofluorescent or hyperautofluorescent just along the border. It is believed that this feature is caused by “heaped up” RPE cells that are dying or near death. This occurrence can be seen in patients diagnosed with AMD and is a clue that GA is present. The autofluorescence may take different patterns such as focal, patchy, banded (nearly continuous thin band around the lesion), or diffuse (areas with increases that go farther out),1 of which the latter 2 are known to have much faster GA progression. (Figure 2)2
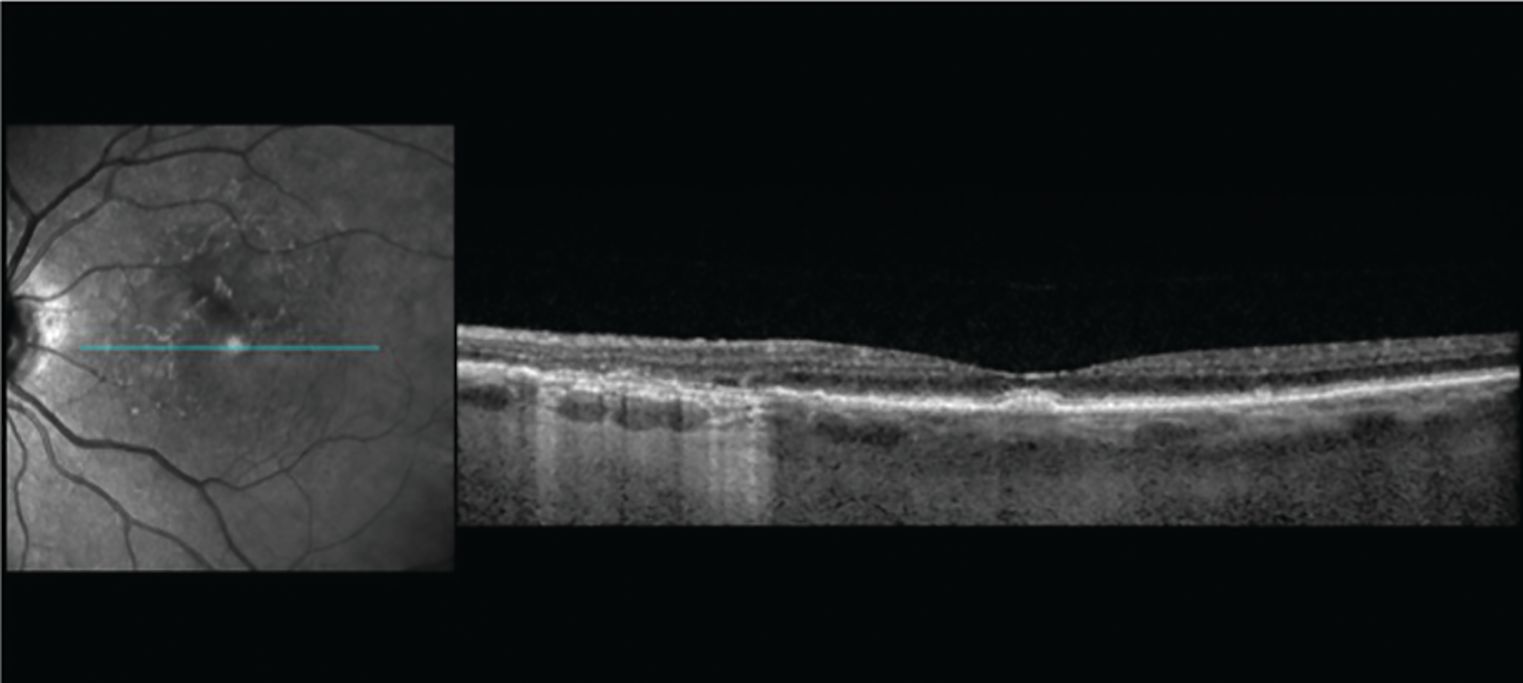
For my patients with AMD and GA, I especially appreciate the high-resolution images obtained with SPECTRALIS. They provide clear details when it comes to hyper-reflective foci and hypertransmission, for example, which represent the early degeneration of the outer retina. (Figure 3)
Figure 3. Early signs of geographic atrophy seen on in the left side of the image, including hyper-reflective foci, wedge defect, and iRORA (incomplete retinal pigment epithelium and outer retinal atrophy). cRORA (complete RORA) is also present.
(Image courtesy of Jeremiah Brown Jr, MD)
Timing of follow-up OCT
When someone has been identified as having GA due to AMD, the lesion appearance and the proximity to the fovea provide more information to help determine treatment and follow-up timing. For example, a patient who has lost vision in 1 eye and has GA in the better-seeing eye should be encouraged to have treatment as soon as possible. I recommend providing these patients with information about therapy and seeing them back within a few months. Clinical trials of the new GA drugs have shown that the longer the patient is treated, the more effective the treatment is in reducing RPE and photoreceptor integrity loss.3 The goal is to save as much of the retina as possible, which is even more critical in patients who have already lost vision in 1 eye.
For patients who have lesions in both eyes but are not immediately affected by them, I typically want to see them back in 4 to 6 months. I share information about GA injections and show them their imaging, advising them to talk it over with their family and consider starting treatment. On their next visit, I will have a deeper, more detailed discussion about the protocols.
In the past, I might have waited a year to see patients with nascent GA, or large drusen with hyper-reflective foci, for their next OCT exam. Now I will have them back in 4 to 6 months to check for progression, informing them that there is now a dry AMD treatment option for which they may be a candidate.
Possibility of wet AMD Development
Through the GA clinical trials, we have learned that the medicines that inhibit the complement pathway confer a higher rate of choroidal neovascularization (CNV) in patients with AMD. The pegcetacoplan injection showed a 12% rate of CNV with monthly treatment and 7% for every other month compared with 3% in control patients.4 Avacincaptad pegol was associated with a 7% CNV rate in the group injected monthly versus 4% in the sham group.5
It is imperative that we let patients know we are watching for this development, and therefore I recommend they have an OCT performed every time they get their injection. If we catch and treat exudative AMD early, the clinical trials reassure us that CNV need not affect their vision. Of note, patients in the trials did not have their GA treatment halted during concurrent wet AMD therapy.
Being positive and proactive
In light of new therapies, we as eye care specialists should be cheerleaders for treatment when we talk to our patients about their options. I believe in being as positive as possible and using images to educate my patients. After a year of getting injections every month or every other month, sometimes patients wonder why their vision is not different. That, we must tell them, is exactly what we want. In other words, I let them know that no news is good news—the fact that nothing is happening is positive.
Unfortunately, everyone who has GA will experience disease progression; therefore, patients should understand that the injections are a preventive treatment. Nevertheless, it is exciting that now we have the first generation of medicines capable of slowing thinning, thereby allowing us to preserve the retina. I explain to patients what this means in practical terms: They can drive or read longer than they would otherwise. I show them OCT and autofluorescence images to let them know what we are looking for.
I think it is very important to continue to counsel all our patients about key lifestyle behaviors. I talk with them about using sunglasses that are labeled for blocking all UV light and advise them to have UV-blocking filters on their eyeglasses. I also educate about the important role of diet and encourage them to include green leafy vegetables, fish, and AREDS 2 supplements. Although the supplements have not been shown to slow GA, they can help to slow progression to wet AMD for those with intermediate AMD and drusen, as per the clinical trial results.6
Conclusion
The approval of 2 drugs for the treatment of GA for the first time is nothing short of a breakthrough in ophthalmology, giving us tools for preserving the retina longer and positively impacting the course of the disease for our patients. Education, attentive and prompt follow-up, and high-resolution OCT have never been more important in caring for our patients with AMD.
Jeremiah Brown Jr, MD
Jeremiah Brown Jr, MD, founded the Brown Retina Institute in 2010 to establish a practice devoted to diagnosing, treating, and researching diseases of the retina and vitreous. In 2022, he joined Retinal Consultants of Texas to expand his research goals.He is the author of numerous peer-reviewed articles on retina diseases. Brown is past president of the San Antonio Society of Ophthalmology. He also serves as a voting member on the FDA Ophthalmic Devices Panel. Brown receives research funding from Genentech, REGENXBIO, Opthea, Outlook, Character Biosciences, and Apellis. He serves on advisory boards for Genentech, Allergan, and Outlook.He is also on the Speaker Bureau for Genentech, Iveric Bio, and Apellis.
REFERENCES
Bindewald A, Schmitz-Valckenberg S, Jorzik JJ, et al. Classification of abnormal fundus autofluorescence patterns in the junctional zone of geographic atrophy in patients with age related macular degeneration.Br J Ophthalmol. 2005;89(7):874-878. doi:10.1136/bjo.2004.057794
Holz FG, Bindewald-Wittich A, Fleckenstein M , Dreyhaupt J, Scholl HP, Schmitz-Valckenberg S; FAM-Study Group. Progression of geographic atrophy and impact of fundus autofluorescence patterns in age-related macular degeneration.Am J Ophthalmol. 2007;143(3):463-472. doi:10.1016/j.ajo.2006.11.041
Heier J, Singh R, Wykoff C, et al. Efficacy of intravitreal pegcetacoplan in geographic atrophy: 24-month results from the phase 3 OAKS and DERBY trials. Paper presented at: Retina Society 55th Annual Scientific Meeting; November 2-5, 2022; Pasadena, CA.
Syfovre. Prescribing information. Apellis Pharmaceuticals, Inc; 2023.https://pi.apellis.com/files/PI_Syfovre.pdf
Patel SS, Lally DR, Hsu J, et al. Avacincaptad pegol for geographic atrophy secondary to age-related macular degeneration: 18-month findings from the GATHER1 trial. Eye (Lond). 2023;37:3551-3557. doi:10.1038/s41433-023-02497-w
Chew EY, Clemons T, SanGiovanni JP, et al; AREDS2 Research Group. The Age-Related Eye Disease Study 2 (AREDS2): study design and baseline characteristics (AREDS2 report number 1). Ophthalmology.2012;119(11):2282-2289. doi:10.1016/j.ophtha.2012.05.027

Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.