
Ultra-wide field imaging shows nonperfusion and leakage independently predict diabetic retinopathy progression, suggesting earlier treatment with anti-VEGF or photocoagulation may prevent complications.

Ultra-wide field imaging shows nonperfusion and leakage independently predict diabetic retinopathy progression, suggesting earlier treatment with anti-VEGF or photocoagulation may prevent complications.

Four-year study shows faricimab in treat-and-extend regimen maintains vision for diabetic macular edema patients with significantly fewer injections over time.

Kapil Mishra, MD, discusses an overview of radiation retinopathy and its challenges in treating uveal melanoma from his presentation "Radiation Retinopathy: Future Strategies,"

Duke professor Sharon Fekrat, MD, discusses AI-driven ophthalmology with smartphone diagnostics and robotic procedures, emphasizing global collaboration and innovative medical research.

According to Dr. Danzig, the DIAMOND trial demonstrates efficacy of OCS-01, a topical drop, in patients with diabetic macular edema.
Jennifer Lim, MD, FARVO, FASRS, discusses her ARVO presentation on sickle cell retinopathy, highlighting improvements in retinal surgery techniques and instrumentation.
The PRISM clinical trial assesses 4D-150 (4D Molecular Therapeutics) in adults with neovascular age-related macular degeneration, also known as wet AMD.
In an analysis of the IRIS database, investigators assessed almost 1,200 eyes that had been treated with faricimab.
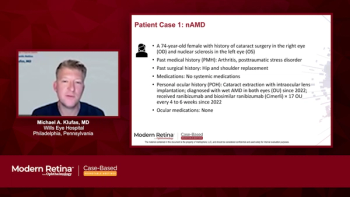
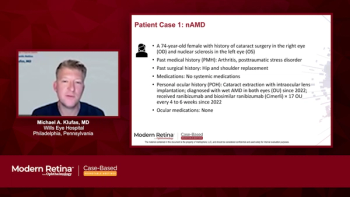
A panelist discusses how a woman aged 77 years with bilateral neovascular age-related macular degeneration (nAMD) demonstrated different responses to treatments between her eyes, showing a superior response to faricimab in her right eye compared with ranibizumab, highlighting how some patients may respond better to specific anti-VEGF agents.
A panelist discusses how a man aged 79 years with long-duration diabetes and treatment-naive diabetic macular edema (DME) responded well to aflibercept 8-mg therapy, progressing from 4-week loading doses to an extended 10-week interval with resolution of macular edema and improved vision from 20/60 to 20/30.
A panelist discusses how a woman aged 74 years with neovascular age-related macular degeneration (nAMD) showed improved disease control and vision in her right eye after switching from ranibizumab to a high-dose aflibercept (8 mg) treatment that successfully extended intervals to 10 weeks.

Abby Markward, MBA, executive director of the ASCRS Foundation and the ASOA, provides a sneak peek of the posterior segment-focused event.

Panelists discuss how longer-acting treatments will enable extended intervals between visits while requiring careful adjustment of monitoring protocols and clinic workflows to balance reduced treatment burden with maintaining adequate disease surveillance.
The 15th annual meeting, taking from March 24–28 in Snowmass, Colorado, will deliver high-impact discussions on macular disease, artificial intelligence in ophthalmology, and breakthrough therapies—plus opportunities for networking on and off the slopes.

Panelists discuss how loading doses remain crucial for treatment-naive patients to achieve rapid disease control, while patients switching therapies may require modified approaches based on their prior treatment response and disease activity.

Panelists discuss how real-world evidence provides crucial insights into treatment effectiveness across diverse patient populations and clinical settings while highlighting challenges in maintaining clinical trial protocols’ stringent adherence and monitoring in everyday practice.

Panelists discuss how both medications demonstrate favorable safety profiles in clinical trials, with aflibercept 8 mg benefiting from extensive 2-mg safety data, while acknowledging the need to monitor intraocular pressure due to increased injection volume, particularly in at-risk patients.

Panelists discuss how faricimab’s dual inhibition of Ang-2 provides additional benefits in vascular stability and inflammation reduction beyond VEGF-A suppression alone, potentially leading to improved durability and treatment outcomes in selected patients.
Panelists explore how the introduction of tyrosine kinase inhibitors (TKIs) could affect the perceived benefits of the port delivery system, as these agents may offer an alternative approach to reducing injection burden while potentially providing broader therapeutic effects.

Panelists discuss how novel intravitreal agents faricimab and high-dose aflibercept 8mg offer potential advantages in treating retinal diseases through their extended durability and dual mechanism of action.

Panelists discuss how faricimab’s bispecific antibody design uniquely targets both VEGF-A and Ang-2 pathways, addressing the complementary role of Ang-2 in vascular destabilization and inflammation in retinal diseases.

Panelists discuss how careful patient selection and management of potential complications - including surgical risks, device-related adverse events, and cost-benefit considerations requiring operating room resources - are crucial factors in successfully implementing the port delivery system in clinical practice.

Panelists discuss how ideal candidates for aflibercept 8 mg include patients with stable disease on current anti-VEGF therapy who seek reduced treatment burden, newly diagnosed patients, and those demonstrating good response to initial loading doses.
Panelists discuss how the port delivery system (PDS) refill procedure, while performed in an office setting, involves a different technique of accessing and replenishing the implant’s drug reservoir through the conjunctiva and requires specialized training compared with standard intravitreal injections.

Panelists discuss how the Port Delivery System (PDS) presents important considerations around adverse effects, patient selection criteria, and adoption challenges including surgical requirements and cost-benefit analyses that must be carefully weighed when integrating this technology into retinal practice.

Dr Jordan Graff highlights key steps in implanting the port delivery system, emphasizing incision and closure techniques with video clips.

Panelists discuss how the phase 3 PULSAR and PHOTON trials demonstrated the efficacy of aflibercept 8 mg through a design comparing 12- and 16-week dosing intervals to the aflibercept 2 mg standard 8-week dosing, with primary end points assessing noninferiority in visual acuity maintenance.
Panelists discuss how patients experiencing frequent anti-VEGF treatment burdens with 4- to 8-week intervals between injections are ideal candidates for PDS as an alternative delivery method.


Panelists discuss how the aflibercept 8 mg higher molecular concentration enables extended durability through increased VEGF binding capacity and longer intraocular drug levels, potentially allowing for less frequent dosing while maintaining efficacy.