- Modern Retina Spring 2022
- Volume 2
- Issue 1
Adapting the inverted internal limiting membrane flap technique in very large macular hole surgery
In the face of the COVID-19 pandemic, the procedure required adjustments.
Reviewed by Eduardo Pérez-Salvador García, MD, PhD.
During the past few months because of the COVID-19 pandemic, the drastic decrease in operating room availability caused the cancellation and postponement of a lot of surgeries. This issue has affected patients with macular holes, bringing about cases of very large, chronic, full-thickness macular holes with a long time of evolution. To achieve the closure and anatomical improvement of these macular holes, we propose the peeling of internal limiting membrane (ILM) and its transposition over the hole, followed by use of a viscoelastic adhesive as a ballast to keep the free flap in the correct position and avoid its migration and displacement from the fovea during fluid-air exchange.
Surgical technique
The previous staining of ILM before the peeling is recommended when performing this technique. Staining will help the correct visualization of the flap, covering the hole during flap transposition and fluid-air exchange when the risk of migration of the flap is higher.
When vitrectomy is combined with phacoemulsification of the lens, the anterior lens capsule can also be used as a free flap in macular hole surgery. In this case, the staining of anterior capsule with dyes, such as as trypan blue, is also advisable. Once it is removed during phacoemulsification, the anterior capsule should be preserved in physiological saline solution (0.9%) until the end of the posterior vitrectomy. After peeling the ILM, position the anterior capsule over the macular hole. Using anterior lens capsule as the flap presents several advantages because we get a bigger, more rigid, more circular, and more regular-shaped flap. These features make the transposition of the flap easier than when the ILM is used. Additionally, this technique eliminates having to peel the ILM in one big piece, which decreases surgical difficulty.
After peeling the ILM, its placement over the macular hole can be challenging because the ILM usually sticks to Eckardt forceps. This problem can be solved by pulling apart the flap with the light probe. Afterward, with the forceps closed, move the ILM and position it over the hole.
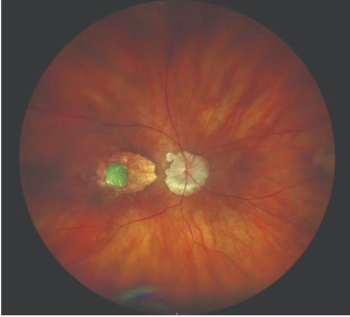
We suggest positioning the flap, anterior capsule, or ILM toward the temporal area of the macula because during fluid-air exchange, the flap tends to move to papilla. When the flap is in the correct position, we apply a viscoelastic adhesive with a silicone-sleeve cannula (Figures 1 and 2). This will keep the free flap in place during fluid-air exchange. The fluid-air exchange should be slow, with exchange pressures lower than 40 mmHg and low vacuum. Remember to put the silicone sleeve of the extrusion cannula over the papilla and be careful not to catch and suck the flap, particularly in the end of the exchange when we take the last fluid from the posterior pole.
Once the fluid-air exchange is accomplished, we should check that the flap is well positioned (Figure 3), which is easily ascertainable if staining had been performed (as previously explained).
Results
This adaptation of the surgery technique of the inverted ILM flap was performed in 5 consecutive patients from January to September. The patients presented with stage 4, long-term evolved, very large macular holes. All of them presented with a size greater than 850 μm, and 4 of them presented with a size greater than 1100 μm. Macular hole mean size was 1208.8 μm. ILM was used as the flap in 3 of the cases, and the anterior lens capsule was used in 2 cases. Viscoelastic adhesive and dye were used in all cases, following the technique exposed. Optical coherence tomography performed 24 hours after surgery in all cases showed the flap was well positioned. Moreover, flap macular hole closure was achieved in all cases.
We have found out that in some of these cases with so much evolution time, some parts of the ILM became fibrosed, usually at the edges of the macular hole. In these cases, we suggest, if possible, using the anterior lens capsule as flap as well as removing the ILM due to the possibility it could stimulate inflammation, which leads to bad results.
Conclusions
Viscoelastic adhesive is a good choice to hold the flap in the correct position, and it avoids the need for the “tuck technique” and its possible mechanical damage to the retinal pigment epithelium (RPE) layer and foveal choroids. Furthermore, it allows us not to keep an attached part of the ILM at the edge of the macular hole to avoid its migration, which is not always possible. It is a simple and cost-effective alternative that has showed no toxic impact on the retina, which can be left in the position.
The use of the anterior lens capsule as flap presents several advantages and could be an especially useful alternative when there is fibrosis of the ILM. We recommend the staining of the flap, regardless of the use of the anterior lens capsule or the ILM.
Both alternatives described in this article consist in autologous procedures and demonstrate the benefits of this kind of procedure. The employment of amniotic membrane as flap, when the use of the anterior lens capsule or ILM is not possible, provides another alternative.
Based on our outcomes, we suggest performing this technique in chronic, long-evolved, full-thickness and persistent macular holes larger than 650 μm.
References
1. Xu Q, Luan J. Internal limiting membrane flap technique in macular hole surgery. Int J Ophthalmol. 2020;13(5):822-831. doi:10.18240/ijo.2020.05.19
2. Benson WE, Cruickshanks KC, Fong DS, et al. Surgical management of macular holes: a report by the American Academy of Ophthalmology. Ophthalmology. 2001;108(7):1328-1335. doi:10.1016/s0161-6420(01)00731-x
3. Fung NSK, Mak AKH, Yiu R, Wong IYH, Lam WC. Treatment of large, chronic and persistent macular hole with internal limiting membrane transposition and tuck technique. Int J Retina Vitreous. 2020;6:3. doi:10.1186/s40942-019-0206-7
Articles in this issue
almost 4 years ago
PDS ushers in a new era in treatment of wet AMDalmost 4 years ago
Emerging treatments for advanced dry AMDalmost 4 years ago
Reshaping retina treatment with faricimabNewsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.