Clinical Trials at the Summit 2023: Is glycoimmunology the next-generation treatment paradigm for GA?
Tarek S. Hassan, MD, FASRS, provides an update on glycoimmunology as a next-generation treatment paradigm for geographic atrophy.
Tarek S. Hassan, MD, FASRS, explores glycoimmunology as the next-generation treatment paradigm for patients with geographic atrophy with Sheryl Stevenson, group editorial director, during the Clinical Trials at the Summit meeting on June 10, 2023, in Park City, Utah. Hassan is a professor of ophthalmology at the Oakland University William Beaumont School of Medicine.
Video transcript
Editor’s note: This transcript has been edited for clarity.
Sheryl Stevenson: We're here with Dr. Hassan, who will be presenting at this year's Clinical Trials at the Summit in Park City, Utah. Welcome to you, Dr. Hassan. We're really intrigued by the title of your talk regarding the next-generation treatment paradigm for geographic atrophy. Can you tell us a little about your presentation?
Tarek Hassan, MD, PhD: Thank you, Sheryl. I appreciate that you asked me to speak for Ophthalmology Times and nice to see you here. Nice to have the opportunity to speak about this. I'm really excited to speak at the Clinical Trials at the Summit meeting about something that I think most of the audience has probably not heard.
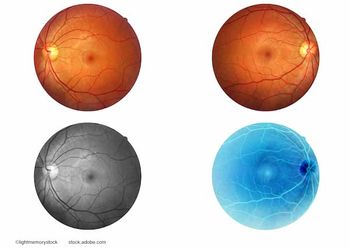
It's an area that is now just exploding across medicine called glycoimmunology where we are literally trying to harness the body's own system of glycosylation, the sugars that we all have on all the cells of our bodies, which serve as many functions, but one of them is to trigger the immune system by binding with certain receptors on immune cells all over our bodies. In our natural state, immune cells of every type have receptors that are called siglecs. They stand for sialic acid like immunoglobulin lectins, but they're receptors. They live on all the immune cells in the body, and they search around all the time and they bind to sialic acids, 9-carbon sugars, that exist on all the cells in our body and because of the appropriate interaction, our immune cells recognize our own cells as self. But if a pathogen or a tumor or some other thing comes in, and has a different glycosylation pattern on their cells, then these receptors on the immune cells recognize them as not self, and attack, initiate an immune reaction.
We have figured out a way to deliver a nanoparticle coated with sialic acids of the specific types that have a high specificity for certain siglecs, which are the receptors on all the immune cells, different ones for different immune cells, such that we can deliver something that binds at a much higher affinity than natural cells to control the behavior on and off of the immune cells. Dry AMD, in particular, and geographic atrophy, in this case, is a disease ultimately of chronic inflammation.
That's why attacking complement has become the new frontier of trying to stop geographic atrophy from companies that have done a great job of bringing their drugs to market. In the end, the best results show something in the order of 20% to 25% maybe reduction from the large pivotal trials of the progression of geographic atrophy, which leaves a very large portion of matched or unresolved progression that we think that we might have the key to. Macrophages in particular microglia are highly involved in the process of geographic atrophy forming and they have exhibited high levels of what are called siglec-7, -9 and -11, specific receptors.
We have a particle called AVD-104, a new molecule which we are now testing, which is highly bound to these receptors, 7, 9, and 11, and are able to modulate the activity of macrophages and microglia which are ultimately the cells that cause geographic atrophy. We can turn them from their activated state. There are different macrophages, the activated M1 or M2a macrophage states and turn them into resolution macrophages, which are the M2c macrophages. In so doing, if we can deliver a molecule, we turn off the attack cells, the macrophage cells, and we put them in almost a state of remission so that they don't continue to eat our own natural retinol and retinal pigment epithelium [RPE] tissue.
As a side benefit, these particular sialic acids that we can deliver and even naturally, actually bind to complement factor H also. It's just because that's a protein binding that occurs anyway. As a sort of secondary mechanism of AVD-104, we actually bind to CFH which reduces C3, and we actually have found that we can block complement factor C3 to a level that is comparable to what has been seen in other studies with other molecules. We present a dual mechanism of action drug that can reduce complement as has been seen by other companies but can also stop the macrophage attack on the retinal tissue, which is ultimately the cause of geographic atrophy. We think we have something super exciting.
It's been done similarly using other receptors that are similar to the siglecs in what are known as T-cell checkpoint inhibitors, like Keytruda and other cancer drugs, which antibodies go to receptors and activate the same inhibitory pathways, but only in T-cells for cancer, and only with antibodies. We've sort of unlocked this potential, where we can use sialic acids, which there are many, and attack all immune cells to turn on those same inhibitory pathways that have been so successful with checkpoint inhibitors. It's really new and exciting. There's a ton of biochemistry and biology that we are learning, and we have to express out to the community.
Our drug has now just been initiated into its first phase 2 trial, just enrolling patients this month. It's part one of the phase 2 trial. Part 2, the larger phase 2 trial, will begin later this year. We've really gone right ahead into the end of the clinic because this mechanism of action is extremely safe. We've seen essentially...we've seen no toxicity at levels much higher than what we intend to use in the human in multiple species, including nonhuman primates. It appears to be extremely safe. Its mechanism of action seems fairly well proven, and it's got a very long duration. We've found this drug in the retinal pigment epithelium and the photoreceptor layer of the retina up to 28 plus days at essentially full dose, which suggests to us that we probably are looking at every 4-to-6-month dosing of this drug, if it all proves to be efficacious. It's very exciting and I'm excited to present it at CTS. I look forward to hearing more from our community, too, as we go forward.
Stevenson: Such a fascinating research topic. What are the key takeaways for the clinician and their patients?
Hassan: We think more is coming. The key takeaway is that complement inhibition has been a wonderful addition to our armamentarium to try to stop the progression of geographic atrophy. It seems as though the majority of that story is still yet to be written and complement inhibition has gotten fairly consistent, good results to this point. It may ultimately represent the minority of what we're trying to get done to actually control this disease.
We may be looking at the areas that are actually attacking the retinal tissue and the photoreceptor layer, specifically, the RPE of the macrophages, that we can maybe pick up a whole lot of that extra 75% that doesn't seem to be reduced with what we currently have. The potential to put dry AMD and geographic atrophy into remission may actually be there.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.