Consensus clinical trial design for the treatment of intermediate AMD
To date, only the onset and enlargement of hyperTDs measured using en-face OCT imaging has been validated as a clinical trial endpoint.
Reviewed by Phillip J. Rosenfeld, MD, PhD
Philip J. Rosenfeld, MD, PhD, Professor of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, Miami, discussed the arrival at a design of a consensus clinical study of intermediate age-related macular degeneration (iAMD) at the Clinical Trials at the Summit 2024 annual meeting on June 9, in Park City, Utah.
Considerations for a Phase 2b trial in iAMD
The general concepts for such a trial should include the following, according toRosenfeld and the members of the Ryan Initiative for Macular Research 2024 and the Classification of Atrophy Meeting #10:
- The Phase 2b study should be designed so it could be used as 1 of the 2 required pivotal Phase 3 studies
- Recognition that the study will likely run for 2 years, but interim analyses before 2 years will help plan the Phase 3 studies
- Interim analyses will be possible between 6 months to 1 year after the trial starts, but it is unlikely that an analysis at 3 months would be informative
- Important to include subjects at high-risk for disease progression, with the caveat being that it might not be possible to modify disease progression in these high-risk patients
- The FDA recommends that the primary endpoint in iAMD trials identify a slowing in the rate of disease progression (continuous endpoint) and not just a decrease in the onset of an event, such as an anatomic or functional endpoint.
OCT endpoints: the value of hyperTDs
Since optical coherence tomography (OCT) imaging is considered the gold standard for following eyes with nonexudative AMD, clinical trial endpoints using OCT imaging are needed to define the onset and rate of disease progression. Of the various OCT features considered as clinical trial endpoints such as incomplete retinal pigment epithelium (RPE) and outer retinal atrophy (iRORA), complete RORA (cRORA), nascent geographic atrophy (nGA), large (persistent) hypertransmission defects (hyperTDs), ellipsoidal zone (EZ) loss, outer nuclear layer thinning, and onset of exudative AMD, only the onset and growth of hyperTDs and progressive EZ loss can be measured as continuous variables to determine the rate of disease progression. To date, only the onset and enlargement of hyperTDs measured using en-face OCT imaging has been validated as a clinical trial endpoint.1
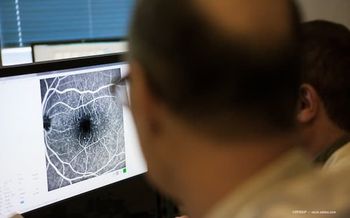
HyperTDs are visualized on en-face OCT imaging derived from dense OCT raster scans.The en-face image is created from a slab positioned 64 microns to 400 microns beneath Bruch’s membrane and is referred to as a sub-retinal pigment epithelium (subRPE) slab. Rosenfeld showed that typical geographic atrophy (GA) appears bright on en-faceOCT images using this subRPE slab because of the choroidal hypertransmission that results wherever the RPE is lost or attenuated. The subRPE slab highlights this hypertransmission and increased reflectance of light from the choroid.1
He demonstrated the onset and progression of hyperTDs in eyes with dry AMD that contain a large drusen burden without evidence of hyperTDs. As these eyes are followed and as the drusen volume increases, one or more hyperTDs form before the collapse of drusen, and these multiple hyperTDs grow and converge to form typical GA. Once the hyperTDs reach a greatest linear dimension on en-face imaging of at least 250 microns, they persist and are referred to as persistent or large hyperTDs. A B-scan through a typical large hyperTD appears similar to cRORA, but the advantage of using the en-face appearance of hyperTDs rather than the B-scan appearance is that the en-face growth of the area can be measured while the growth of cRORA on B-scans is limited to the horizontal dimension. The onset of large hyperTDs serves as the point of no return as additional hyperTDs form and grow, and the total growth of the hyperTD area serves as the clinical trial endpoint.
Longitudinal assessment of drusen volume and hyperreflective foci area in the 5-mm central circle
In designing clinical trials, Rosenfeld emphasized the importance of knowing the natural history of disease progression in eyes with certain high-risk features so the likelihood of disease progression can be predicted within 2 years. By studying 171 eyes with iAMD over a mean follow-up of 60 months, his group found that eyes with a central drusen volume of at least 0.22 mm3 were likely to progress within 2 years. In addition, they found that the likelihood of disease progression increased with evidence of hyperpigmentation on examination or hyperreflective foci on OCT imaging, in association with a drusen volume of at least 0.22 mm3. These findings from Rosenfeld’s natural history study are currently under review at the American Journal of Ophthalmology.
Consensus clinical trial guidelines:
Enroll high-risk drusen eyes with any evidence of hyperreflecive foci
Evidence of a central drusen volume of at least 0.2 mm3 or larger
No evidence of persistent hyperTDs
Randomize about 100 eyes into each group (treatment vs. sham); 100 eyes ensures that an adequate number of eyes will develop hyperTDs within 1 year in the placebo group
Plug-and-play clinical trial design for studying iAMD
Rosenfeld explained that the proposed clinical trial design could be used for any therapy that might slow disease progression from iAMD to late AMD.The consensus inclusion criteria are patients at least 60 years of age and eyes with iAMD that are at high risk for disease progression, with an OCT drusen volume threshold ≥ 0.22 mm3 and more than 1 hyperreflective foci in the macula.
In the first year of the study, the hyperTDs form in the placebo control arm; a sneak peak at the onset of hyperTDs in the active and control arms within 6 months to 1 year after the start of the study should provide an indication if the treatment is slowing disease progression.However, the actual treatment efficacy will be determined in the second year of the study when the overall growth rate of hyperTDs is compared between the placebo and different treatment arms. Of note, the growth of hyperTDs depends not only on the onset but the growth of individual lesions. This clinical trial design was accepted by the FDA for a Phase 2b study.
While the growth rate of large hyperTDs is the primary endpoint in the study, other noteworthy secondary endpoints include the onset of new large hyperTDs/eye, onset of macular neovascularization, change in drusen volume, change in hyperreflective foci, and the changes in functional tests, such as best-corrected visual acuity, low-luminance visual acuity, and results of targeted microperimetry.
Take-home points
For an iAMD study, the following guidelines apply: enroll high-risk eyes likely to progress within 2 years; OCT imaging will define the primary endpoint; the primary endpoint is the growth rate of large hyperTDs over 2 years; the 1-year interim analysis will be the onset of hyperTDs; and a successful randomized, double masked, placebo-controlled Phase 2b should serve as one of two phase 3 clinical trials.
Reference
1.Liu J, Shen M, Laiginhas R, et al. Onset and progression of persistent choroidal hypertransmission defects in intermediate age-related macular degeneration: a novel clinical trial endpoint. Am J Ophthalmol.2023;254:11-22; doi: 10.1016/j.ajo.2023.03.012
Presentation
Rosenfeld PJ. Real-World Experience with Intravitreal Pegcetacoplan for the Treatment of GA. Presented at the Clinical Trials 2024 at the Summit; June 9, Park City, Utah. Session: Imaging and Functional Biomarkers for Clinical Trials
Phillip J. Rosenfeld, MD, PhD
E: prosenfeld@med.miami.edu
Rosenfeld is Professor of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine, Miami. He has financial interests in this subject matter. Rosenfeld serves as an advisor to Abbvie, Annexon, Apellis, Bayer Pharmaceuticals, Boehringer-Ingelheim, Carl Zeiss Meditec, Genentech/Roche, InflammX Therapeutics, Ocudyne, Regeneron Pharmaceuticals, and Unity Biotechnology. He also has equity interest in Apellis, InflammX, Ocudyne, and Valitor.
He is an advisor for Apellis and holds equity in Apellis.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.