Double trouble: Handling retinal detachment in the setting of global trauma
Leanne Clevenger, MD, described a case that highlights varying approaches and protocols for addressing a complex case of retinal detachment repair in a patient with trauma to the globe.
Reviewed by Leanne Clevenger, MD
Leanne Clevenger, MD, described a case that highlights varying approaches and protocols for addressing a complex case of retinal detachment repair in a patient with trauma to the globe. Clevenger, from the Cleveland Clinic, Cole Eye Institute, Cleveland, described the case at the Retina Fellows Forum in Chicago.
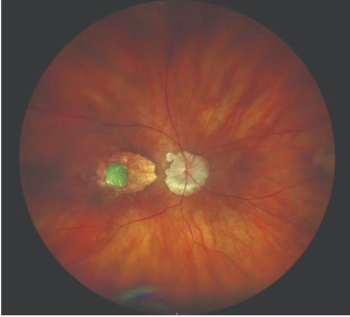
A 71-year-old man presented 2 days after sustaining blunt trauma to the right eye. The preoperative examination was significant for counting fingers vision at near and hypotony with a dense vitreous hemorrhage; the intraocular pressure (IOP) was 2 mmHg.
A slit-lamp examination showed 1+ corneal Descemet folds, a very deep anterior chamber with trace hyphema, and a nuclear sclerotic cataract. The posterior examination showed a vitreous hemorrhage, and a possible retinal detachment temporally, but visualization was challenging. At this point in the evaluation, Clevenger reported that there was great concern for a ruptured globe. Further exploration was needed.
The initial evaluation also showed a 15-mm zone III scleral laceration that was repaired; a scleral buckle was positioned over the laceration. On postoperative day 1, the visual acuity was hand motions and the IOP increased to 11 mmHg. Because of the vitreous hemorrhage, the intraocular view was hazy; the retina was observed to be grossly attached. B-scan ultrasonography showed denser vitreous opacities inferiorly and the grossly attached retina. Another evaluation was planned for 5 days later.
One week later, the patient underwent a pars plana vitrectomy. Careful vitreous base dissection was required in the setting of the dense vitreous hemorrhage, Clevenger described, and the retina was ultimately flattened using perfluoro-n-octane and stabilized with a perfluoropropane tamponade.
Two months after the vitrectomy, the vision was 20/100 despite macular atrophy on optical coherence tomography. Cataract progression was seen.
“This was a challenging trauma case in which a staged repair was more helpful than a single surgery,” Clevenger concluded.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.