What photobiomodulation may mean for patients with dry AMD
Find out how the LIGHTSITE I results may pave the way for a new treatment approach.
Photobiomodulation (PBM) may be a promising therapy for patients with dry age-related macular degeneration (AMD), which currently has no proven effective treatment.
The investigators of the LIGHTSITE I study, which evaluated the effectiveness of PBM, explained that the treatment involves “targeted use of selected wavelengths of visible light to near-infrared light (500–1000 nm) to produce beneficial cellular effects leading to improved outcomes at the cellular, systemic, and clinical level in a wide range of disease states.”
Several clinical studies have shown that the technology may be useful to treat ocular diseases including amblyopia, retinitis pigmentosa, and AMD. Regarding the last, the investigators of the current study, led by first author Samuel N. Markowitz, MD, cited a study in which laser diode treatment applied to the macula improved visual acuity (VA) in subjects with dry and wet AMD.1 Thereafter, two Toronto and Oak Ridge PBM Studies for Dry Age-Related Macular Degeneration (TORPA I and II) reported clinical (improvements in best-corrected VA [BCVA] and contrast sensitivity [CS]) and anatomic (reductions in drusen volume) benefits after PBM in patients with dry AMD.2,3
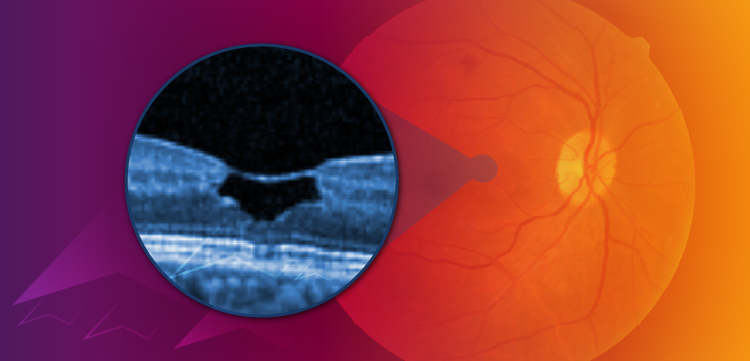
Based on these early studies, the authors hypothesized that PBM may have a therapeutic role in dry AMD, a condition that is characterized by mitochondrial dysfunction, oxidative stress, and inflammation within the retinal pigment epithelial cell layer.
LIGHTSITE I Study
The prospective, randomized, double-masked pilot study included 30 subjects (46 eyes) treated with the Valeda Light Delivery System (LumiThera Inc.). The subjects underwent two series of treatments (a series is a total of 9 treatments over 3–4 weeks) over the 1-year study course. The active treatment included three distinct wavelengths in the yellow (590 nm), red (660 nm), and near infrared (NIR) light (850 nm) range; the sham treatment was an approximate 100 times reduction in treatment fluence compared with the PBM mode and did not include the NIR light.
Outcome measures included the BCVA, CS, microperimetry, central drusen volume and drusen thickness, and quality of life assessments. The investigators reported their results in Retina.4
Fifteen patients were randomized to the PBM group and 15 to the sham group. The mean patient age was 76 years and the mean duration of AMD was 78 years. Most patients had intermediate to advanced dry AMD based on the Age-Related Eye Disease Study categories 3 and 4, 30.4% and 67.4%, respectively, and most eyes had geographic atrophy (73.9%).
Patients treated with PBM had a mean increase in the BCVA of about 4 letters immediately after each treatment series at months 1 and 7. The BCVA in about 50% of the PBM-treated patients improved by 5 letters or more compared to 13.6% in the sham group at month 1. PBM-treated patients who were considered high responders, defined as improving by 5 or more letters at month 1, had an increase of 8 letters after the first treatment, which was significant (P<0.01), and had earlier stages of AMD. The treatment began to lose its peak effectiveness just before the scheduled retreatment at month 6.
The investigators also reported significant (P<0.05) improvements in CS, the volume and thickness of the central drusen, and patient quality of life.
In commenting on the results, the investigators said, “…the LIGHTSITE I results may pave the way for a new treatment approach, expanding the field of PBM into the ocular world to combat a debilitating disease with limited patient options. From a clinician standpoint, the treatment may provide an option to their patients to address the disease early, improve visual outcomes, and potentially slow the progression of the disease.”
Due to these encouraging results, larger multi-center studies are now being conducted by LumiThera, Inc., in Europe and the US.
Clark Tedford, PhD, is an employee of LumiThera, Inc., the study sponsor. The study was partially supported by the National Institutes of Health, National Eye Institute Grant #3R43EY025508-01S1.
References
Ivandic BT, Ivandic T. Low-level laser therapy improves vision in patients with age-related macular degeneration. Photomed Laser Surg. 2008;26:241–245.
2. Merry GF, Munk MR, Dotson RS, et al. Photobiomodulation reduces drusen volume and improves visual acuity and contrast sensitivity in dry age-related macular degeneration. Acta Ophthalmol. 2017;95:e270–e277.
3. Merry G, Dotson R, Devenyi R, et al. Photobiomodulation as a new treatment for dry age related macular degeneration: results from the Toronto and Oak Ridge photobiomodulation study in AMD (TORPA). Assoc Res Vis Ophthalmol. 2012; 53:2049.
4. Markowitz SN, Devenyl RI, Munk MR, et al. A double-masked, randomized, sham-controlled, single-center study with photobiomodulation for the treatment of dry age-related macular degeneration. Retina. 2020;40:1471-1482.
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.