Gaining a greater understanding of AMD
Why investigators are considering AMD to be a disease spectrum rather than a single disease.
Reviewed by Monika Fleckenstein, MD.
A recently published review article on age-related macular degeneration (AMD) presents a comprehensive discussion of current knowledge regarding the disease state, raises important questions to be addressed in future research, and underscores the idea that AMD is not a single entity but instead represents a disease spectrum with distinct phenotypes that appear to have different underlying risk factors and pathogenic pathways.
The 25-page paper1 was written by invitation from the journal’s editors and represents joint efforts by an international expert panel organized by Emily Y. Chew, MD, PhD, director of the Division of Epidemiology and Clinical Applications at the National Eye Institute at the National Institutes of Health in Bethesda, Maryland. The paper covers epidemiology; mechanisms/pathophysiology; diagnosis, screening, and prevention; management; and quality of life, and it cites 280 references.
Related: Age-related macular degeneration: treatment overview
Monika Fleckenstein, MD

Monika Fleckenstein, MD, a professor of ophthalmology at John A. Moran Eye Center at the University of Utah in Salt Lake City, is the first author of the work. She told Modern Retina™ that there have been several recent review articles on AMD but that she believes the paper stands out for the depth and breadth of the information it contains.
“Although our paper, which is a review article, does not present new original research, we believe it highlights some important new concepts about AMD and topics for future investigations,” she said.
Related: Ray-tracing IOL modeling in AMD patients
Moreover, Fleckenstein added that her team believes the global overview of AMD provided in their paper will be useful for all ophthalmologists, ophthalmologists in training, and physicians in other fields of medicine in addition to anyone with a special interest in AMD.
“We hope that our emphasis on the idea that AMD comprises diverse pathological conditions will be thought provoking for basic and clinical scientists as they plan new research that ultimately will lead to improved care and better quality of life for patients with AMD,” she added.
Rethinking AMD
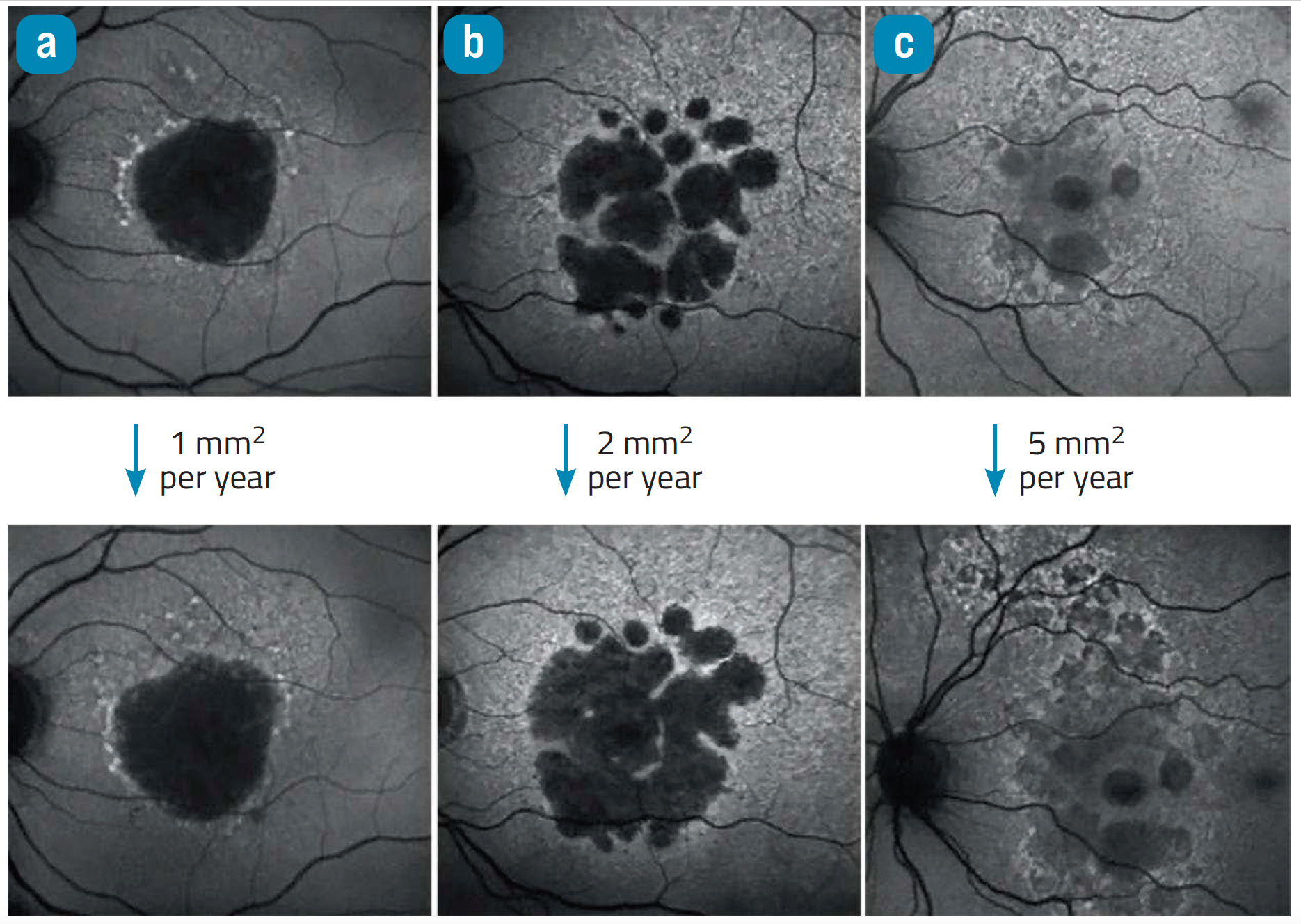
Differential enlargement rates of GA. Serial fundus autofluorescence images of eyes with GA. a] GA lesion with a progression rate of 1 mm2/year and only a few disseminated spots of increased FAF. b] A lesion with a progression rate of 2 mm2/year. In this eye, there is a widespread fine granular FAF signal surrounding the atrophic lesion. c] An eye with a trickling GA phenotype showing the fastest progression. The FAF signal is typically garish in the area of atrophy compared with the other GA subtypes, and the lesion is multilobular, surrounded by extensive reticular pseudodrusen. geographic atrophy = GA; fundus autofluorescence = FAF (Copyright: adapted from REF2)
Fleckenstein pointed out that when the article was solicited, the journal editors asked that it describe a model of AMD. However, complying with this request challenged the writing group because the exact interactions of pathophysiological events that may culminate in different AMD types remain to be elucidated.
“We know there are different phenotypes and stages in this bucket of AMD, and because of accumulating evidence, we are more and more convinced there are different dominant mechanisms for their development,” Fleckenstein said.
Related: Protecting mitochondria with elamipretide
For example, she noted that current information indicates the risk factors for the development of geographic atrophy differ from those associated with progression of the atrophic lesions. Knowledge of these differences is important for researchers, as it indicates a need to focus on different targets for preventive versus therapeutic interventions.
In discussing neovascularization in AMD, the paper highlights new concepts and terminologies that have emerged thanks to clinico-pathological correlations that have been refined through advances in imaging techniques. First, the paper uses the term macular neovascularization (MNV) rather than choroidal neovascularization based on the fact that not all neovascularization in the area of the macula arises from the choroid.
Related: Gene therapy for nAMD maintains vision with single injection
In addition, the article reviews evidence of different types of MNV, some of which seem to protect against AMD progression.
“This latter concept was first put forth decades ago by histopathologists but has only recently gained full attention because newer imaging technologies have enhanced our ability to visualize different subtypes of MNV in vivo,” Fleckenstein said. “Indeed, several studies implementing high-resolution retinal imaging have shown that rates of dry AMD progression differ depending on the presence of certain MNV subtypes.”
Fleckenstein added that the observations may lead to the identification of new therapeutic targets and also arguments against interventions that aim to eliminate all MNV.
Consensus on terminologies
One goal of developing new consensus terminologies for distinct manifestations of AMD is to provide a complete view of pathological changes that occur in the disease.
“The use of common terminology for phenotypic features is important if we want to be able to compare findings from different studies,” Fleckenstein explained.
Related: Laser imaging system may offer early detection, treatment for eye diseases that cause blindness
She noted, however, that it is a task not easily done. For example, although the term MNV recognizes the fact that not all AMD-related neovascularization originates from the choroid, it does not account for the fact that AMD can also be associated with neovascularization in the peripheral retina, Fleckenstein explained.
“It became clear to me while working on this project that it is not always possible to find all-inclusive terms that also reflect the range of experts’ opinions,” she said.
Related: Outlook is bright for telemedicine in ophthalmology
Fleckenstein concluded that even if a group comes to a consensus about a particular classification system or preferred term, other specialists in the field may not agree.
“But it is the open-minded discourse that will advance our field,” she noted. “And we also have to realize that terminologies are always subject to flux as new information emerges.”
Monika Fleckenstein, MD
E: monika.fleckenstein@hsc.utah.edu
Fleckenstein receives grants from Heidelberg Engineering, Genentech/Roche, Novartis, and Optos; personal fees from Bayer, Heidelberg Engineering, Genentech/Roche, and Novartis; and nonfinancial support from Carl Zeiss Meditech, Heidelberg Engineering, and Optos outside the submitted work.
References
1. Fleckenstein M, Keenan TDL, Guymer RH et al. Age-related macular degeneration. Nat Rev Dis Primers. 2021;7(1):31. https://doi.org/10.1038/ s41572-021-00265-2
2. Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, Henry EC, Ferrara D. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018;125(3):369-390. doi: 10.1016/j.ophtha.2017.08.038. Epub 2017 Oct 27. PMID: 29110945
Related Content: Wet AMD Viewpoint | AMD
Newsletter
Keep your retina practice on the forefront—subscribe for expert analysis and emerging trends in retinal disease management.